Tackling High Blood Pressure: A Case for CCG Action
This slide deck prepared by the Clinical Commissioning Group (CCG) provides key insights on addressing high blood pressure to reduce mortality and healthcare costs. Highlights include the impact of high blood pressure on health systems, national leadership efforts, action plans for prevention, detection, and management, and resources for supporting local initiatives. The presentation emphasizes the importance of tackling high blood pressure, which affects a significant portion of the population and contributes to various chronic conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Tackling high blood pressure A case for CCG action Clinical Commissioning Group (CCG) slide deck prepared 18/12/2015
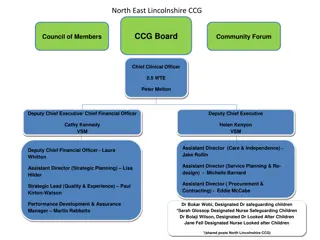
Background Public Health England supports a new programme of work on tackling high blood pressure As part of this we are working to support local to develop leadership around high blood pressure. Our resource hub gathers key materials to support service planning and deliver This slide set is intended to support colleagues working in Clinical Commissioning Groups to make the case for a focus on high blood pressure within their organisation This slide deck is intended to facilitate a discussion about prioritising prevention, detection and/or management of high blood pressure locally 2 Tackling high blood pressure
Introduction High blood pressure leads to costly and disabling conditions including stroke, heart failure, heart attack, chronic kidney disease and vascular dementia Tackling high blood pressure is therefore a major opportunity for CCGs to reduce premature mortality and save on health and social care spending 12 national organisations including Public Health England and NHS England are leading new action on this issue This presentation sets out key insights and evidence from that work, to assist local teams in discussing how to improve the prevention, detection and management of high blood pressure 3 Tackling high blood pressure
Contents Why tackle high blood pressure Impact on health system National performance Local performance New national leadership High blood pressure action plan Prevention Detection Management Resource hub Healthier Lives Hypertension Atlas Future plans 4 Tackling high blood pressure
Why tackle high blood pressure High blood pressure affects more than 1 in 4 adults in England It is the one of the leading risk factors for premature death and disability People from the most deprived areas are 30% more likely than the least- deprived to have high blood pressure Directly addresses NHS Outcomes Framework1.1 under 75 mortality rate from cardiovascular disease and wider Quality and Outcomes Framework (QOF) and local performance measures Improvement is achievable: Adults with high blood pressure diagnosed and controlled 37% England s Top CCG (South West Lincolnshire) Canada average 66% England average 56% 5 Tackling high blood pressure
Global Burden of Disease: England results Dietary risks Tobacco smoke High body-mass index High systolic blood pressure Alcohol and drug use HIV/AIDS and tuberculosis Diarrhea, lower respiratory & other common infectious diseases Neglected tropical diseases & malaria Maternal disorders Neonatal disorders Nutritional deficiencies Other communicable, maternal, neonatal, & nutritional diseases Neoplasms Cardiovascular diseases Chronic respiratory diseases Cirrhosis Digestive diseases Neurological disorders Mental & substance use disorders Diabetes, urogenital, blood, & endocrine diseases Musculoskeletal disorders Other non-communicable diseases Transport injuries Unintentional injuries Self-harm and interpersonal violence Forces of nature, war, & legal intervention High fasting plasma glucose High total cholesterol Low glomerular filtration rate Low physical activity Occupational risks Air pollution Low bone mineral density Child and maternal malnutrition Sexual abuse and violence Other environmental risks Unsafe sex Unsafe water/ sanitation/ handwashing 0% 1% 2% 3% 4% 5% 6% 7% 8% 9% 10% 11% 12% Percent of total disability-adjusted life-years (DALYs) 6 Tackling high blood pressure
Impact on health system High blood pressure accounts for approximately 12% of all GP consultations Estimated 1bn drug costs for high blood pressure per year Diseases caused by high blood pressure cost the NHS over 2bn every year (~ 10m per CCG) stroke 850m coronary heart disease 750m vascular dementia 320m chronic kidney disease 200m Additional cost of social care 7 Tackling high blood pressure
National performance Positive change in last decade - slightly lower population average blood pressure ( 3mmHg systolic), 2 million people newly identified, 10% more on treatment achieving control), however: Significant variation between CCGs (average BP control 61-94% / average proportion of hypertensives identified 37-66%) between income groups (30% more with hypertension in most-deprived areas versus least) 8 Tackling high blood pressure
Local performance NOTE TO PRESENTER: YOU MAY WISH TO INCLUDE LOCAL DATA FROM: Your CCG s cardiovascular (CVD) intelligence pack, available at http://www.yhpho.org.uk/ncvinintellpacks/Default.aspx see slides 11-19 on hypertension, which are fully formatted for use Your CCG s profile on the healthier lives: hypertension site, available at http://healthierlives.phe.org.uk/topic/hypertension data can be downloaded for all high blood pressure indicators by searching your CCG name, then selecting download data via the link at data can also be viewed in interactive map form, and comparisons made with similar CCGs, more details on how to use this tool on the about the data page the bottom left 9 Tackling high blood pressure
New national leadership Since 2014, England s Blood Pressure System Leadership Board (a cross- sector group) has overseen a programme of work improve the prevention, detection and management of high blood pressure, and reduce health inequalities Published in November 2014 Tackling high blood pressure: from evidence into action 10 Tackling high blood pressure
High blood pressure action plan Intended to support partners at all levels to focus upon the work that will make the biggest impact in tackling high blood pressure Contains advice specifically for NHS commissioners Draws on the best evidence (including new economic analysis) and professional judgment of our group to: Recommend most pressing issues on blood pressure pathway to address demonstrate roles for a wide range of organisations to achieve this set out what key partners have already pledged to do in support of our ambition Overarching themes: Tackling inequalities: identifying approaches and targeting to achieve this Partnership: need system leadership at all levels across government, health system, voluntary sector and beyond Local leaders: change and implementation is influenced and driven by local professionals www.gov.uk/government/publications/high-blood-pressure-action-plan 11 Tackling high blood pressure
Prevention (1 of 2) High blood pressure is preventable, and risk of cardiovascular disease is reduced down to a threshold of 115/75mmHg Prevention Key risk factors include excess weight/salt/alcohol, physical inactivity 15% reduction in population salt intake achieved in last decade seen as main contributor to lower population blood pressure ( 3mmHg systolic) Detection Over ten years, an estimated 45,000 quality adjusted life years could be saved, and 850m not spent on related health and social care, if England achieved a 5mmHg reduction in the average population systolic blood pressure Management 12 Tackling high blood pressure
Prevention (2 of 2) Key areas of focus reducing salt consumption and improving overall nutrition at population-level improving calorie balance to reduce excess body weight at population-level Prevention personal behaviour change on diet, physical activity, alcohol and smoking, particularly prompted through individuals regular contacts with healthcare & other institutions Detection Potential opportunities for CCGs integrate prevention and lifestyle modification into clinical care pathways, eg, physical activity, healthy eating, weight management, sensible drinking, smoking cessation Management support behavioural change training for all healthcare professionals to enable effective conversations about healthy lifestyle 13 Tackling high blood pressure
Detection (1 of 3) Vast majority of testing occurs in primary care. In addition: >1.4m NHS Health Checks per year (age 40-74) Voluntary sector (e.g. Know Your Numbers campaign >100,000 tests/year) Pharmacy (e.g. Lloydspharmacy >65,000 tests/year) Validated self-monitoring devices at low cost Testing advisable at least every five years, more frequent re- testing for those with high-normal blood pressure Diagnosis never based on a single test, normally followed by ambulatory (24 hour monitor) or home testing Over ten years, an estimated 7,000 quality adjusted life years could be saved, and 120m not spent on related health and social care costs, if England achieved a 15% increase in the proportion of adults who have had their high blood pressure diagnosed Prevention Detection Management 14 Tackling high blood pressure
Detection (2 of 3) Key areas of focus more frequentopportunistic testing in primary care, achieved through using wider staff (nurses, pharmacy etc.), and integrating testing into the management of long term conditions Prevention improving take-up of the NHS Health Check, a systematic testing and risk assessment offer for 40-74 year olds Detection targeting high-risk and deprived groups, particularly through general practice records audit and outreach testing Management 15 Tackling high blood pressure
Detection (3 of 3) Potential opportunities for CCGs identify the local size and distribution of the shortfall in detection and review testing provision in light of this (links to CCG five year planning on reducing avoidable mortality) Prevention consider the case for investment in enhanced community pharmacy services to provide better information and support about BP management introduce opportunistic screening in some areas use the medicines use review to review the blood pressure of those on anti-hypertensives and others at high risk of developing high blood pressure Detection Management Support healthcare staff to refresh skills on accurate blood pressure testing and effective results communication, including via risk communication tools e.g. QRiskII and JBS3 heart age 16 Tackling high blood pressure
Management (1 of 3) NICE recommend lifestyle treatment for all with hypertension with good adherence can achieve dramatic blood pressure reduction Prevention Drug therapy for all over 160/90mmHg and many below with other risks. Four-step approach to incremental drug treatment set out by NICE. 80% of people require two or more agents to achieve blood pressure control Detection NICE treatment target (for adults under 80 years) 140/90mmHg Over ten years, an estimated 7,000 quality adjusted life years could be saved, and 120m not spent on health and social care, if England achieved a 15% increase in the proportion of adults on treatment controlling their blood pressure to 140/90mmHg or below Management 17 Tackling high blood pressure
Management (2 of 3) Key areas of focus Prevention local leadership and action planning for system change, to tackle particular areas of local variation, and achieve models of person-centric care health professional support (communication, tools & incentives) to bring practice nearer to treatment guidelines where this falls short Detection support adherence to drug therapy and lifestyle change, particularly through self-monitoring of blood pressure and pharmacy medicine support Management 18 Tackling high blood pressure
Management (3 of 3) Potential opportunities for CCGs promote and support clinical leadership for improvement by GPs, nurses and pharmacists Prevention support whole system action planning for primary care to implement NICE guidance particularly step-wise treatment increasing number of agents lifestyle changes to reach control regular review of hypertensive patients full assessment and initiation of BP treatment in those at high CVD risk Detection embed management of high blood pressure within communications about long term conditions Management support use of the Patient Activation Measure, and commission services in response to findings to raise activation optimise access to care of people from marginalised groups 19 Tackling high blood pressure
Resource hub PHE wants to support local leadership in tackling high blood pressure, and has gathered resources in one hub to help those planning and delivering high blood pressure services and initiatives Resources include data, guidance, tools, case studies and examples of emerging practice The PHE team welcomes feedback and ideas for new resources to include, particularly any local case studies please email bloodpressure@phe.gov.uk www.gov.uk/high-blood-pressure-plan-and-deliver-effective-services-and-treatment 20 Tackling high blood pressure
Healthier Lives variation atlas Risk and prevention Detection High risk groups Care LA CCG GP healthierlives.phe.org.uk/topic/hypertension 21 Tackling high blood pressure
The future What is our role in tackling high blood pressure? ? What will we focus on ? Who will we work with ? How will we measure our impact 22 Tackling high blood pressure