Subcommittee on Guidance for Claims Examiners: Medical Evidence Evaluation
Subcommittee on Toxic Substances and Worker Health is tasked with reviewing and evaluating materials for claims examiners in assessing medical claims. The subcommittee encountered issues with determining valid medical information, lack of training on specific toxicants, and challenges in sending cases to relevant bodies. Recommendations include better access to publications on causation, addressing deficiencies in evidence evaluation, and improving CE training. Requests for information from DOL and focus group creation for CEs were also noted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
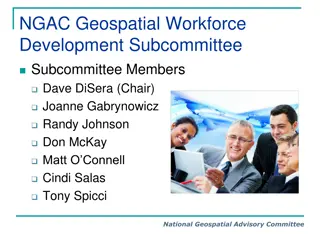
Advisor Board on Toxic Substances and Worker Health Subcommittee on Guidance for Claims Examiners: Weighing the Medical Evidence
Members of Subcommittee Victoria Cassano, Chair Les Boden Steve Markowitz Duronda Pope Ken Silver Faye Vlieger
Task: Review and evaluate and make recommendations pertaining to: the materials available to assist CE s in determining the development and adjudication of medical claims. the logic process used by the CE s in determining what medical information was valid and what was not the training materials available on specific toxicants outside of the SEM and make recommendations
First Meeting: 12 July 2016 Primary Tasks Define Issues and Scope of area Define the data and information needs Draft and initial work plan Reviewed the procedure manual since this is the primary sourse of information for the CE s
Results of review Language regarding the use of medical information from the Former Worker Program In cases going to the CMC, all submitted medical evidence should go to the CMC, not just that which the CE determines to be valid There are publications and consensus documents available which provide better information on causation and outcome, but that it is not the CE s place to parse this information Problems with types of medical evidence utilized to determine a diagnosis Affirmative assistance, CE may not be aware of the medical information needed to adequately adjudicate the claim Issues with the restrictive reasons for sending a case to an IH or a CMC
Meeting 2: 13 September 2016: Review Questions to DOL and requests for information Consensus documents from IARC, National Toxicology program, and other research bodies These should be available to the CE in some form, the claimant does not have the expertise to review these, and they may be ignored if submitted DOL stated only medical evidence that CE determines to be relevant goes to CMC- we did not feel that the CE had the expertise to determine what was relevant Deficient evidence referring to wage loss: we do not believe that the treating physician can make this determination We really wanted to know how the CE is trained to weigh medical evidence . We found that most of the training is on the job usually by a more senior CE; how are they trained to evaluate the validity of medical report Requested to form a focus group of CE s that we could sit with and discuss the development of a claim Requested the training materials available to the CEs besides the procedure manual Requested Part E claims to review specifically from the 14 priority areas
Review of Part B cases TEMPLATE FOR EVALUATING CLAIMS FOLDERS 1. What is the original contention of the claimant? a. Is the original contention (i.e. his document not the SOC) of the claimant available to review? b. Are all the contentions of the claimant addressed by the statement of case? c. Is the Occupational history questionnaire available in the file? 2. Is there a definitive diagnosis? a. Is the diagnosis supported by objective medical evidence? b. Are there alternative diagnoses possible c. Was the diagnosis accepted by the Claims examiner? i. Why or why not? ii. Was this a reasonable decision 3. Were all exposure that might have caused the claimed condition evaluated? 4. Did the treating physician provide a medical opinion regarding causation? a. Was it well rationalized? b. Was the medical opinion from the treating provider accepted by claims examiner? i. Why or why not? 5. Was the claim referred to an industrial hygienist? a. Why or why not? b. Was this decision appropriate? c. If referred did the Industrial hygienist provide a reasoned explanation for decisions regarding exposure? d. Did the claims examiner utilize the information from the Industrial Hygienist appropriately? 6. Was the claim referred to a contracted medical consultant (CMC) a. If not, why? b. Was this decision reasonable? Why or Why not? 7. If referred to CMC, was the CMC given all relevant information to the case? 8. Did the CMC provide a rationalized opinion regarding the nexus between exposures and disease? a. What information, sources, facts were used to develop the medical opinion? b. Was the utilization of resources adequate? c. Was the interpretation of the information appropriate? 9. Was the claim accepted or denied? a. On what basis? b. Was this a reasonable determination? Why or why not? 10. If the case was referred to a final adjudication board, follow the appropriate sections of the above template to review the appealed decision.
Results Claims folders incomplete Only had the medical information and the Statement of case by the CE Did not have the EE1 which shows the actual contention of the claim by the employee Did not have the employees Work history (EE3) In many cases did not have the Occupational health questionnaire If a medical opinion was provided with clear rationale for causation by treating physician, then claim had a better chance of being accepted Several cases where alternative medical diagnoses may have been considered (sarcoidosis versus berylliosis) If worker not in a working group for which exposure is already conceded, the claim is denied. (Truck driver at uranium mine, not a miner = not exposed) Claims denied simply on lack of radiologic evidence regardless of treating physicians diagnosis
To be accomplished in near future CE forum: Discuss how they develop claims, More complete review of part E claims Evaluation of training materials and recommendations for improved training materials for Ces Investigate how to operationalized causation, contribution and aggravation
Recommendations Develop better training materials that provide some standardization across the process for the 14 priority areas All medical evidence should be submitted to the CMC, not just that which is determined to be relevant by CE. Other evidence of exposure must be utilized other than the SEM for determining work-relatedness and IH should evaluate on case by case basis where necessary Consider presumptions