Step-Wise Approach in ICU Management of a Patient in Respiratory Distress
An intensivist outlines a systematic approach for managing an acutely unstable patient in respiratory distress in the ICU. The process includes clinical assessment, noninvasive ventilation options, considerations for vital organ functions, and potential pitfalls to avoid. Emphasis is placed on differentiating between diagnosis and clinical status evaluation to prevent complications.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Step Wise Approach in ICU Management of a Patient in Respiratory Distress: An Intensivist s Assessment Omer Mirza, MD, Intensivist - Covenant HealthCare
A THING TO REMEMBER An education isn't how much you have committed to memory, or even how much you know. It's being able to differentiate between what you know and what you don't know. Anatoly France.
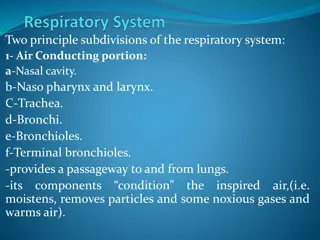
INTRODUCTION Clinical assessment of the acutely unstable patient. Noninvasive ventilation. High flow nasal cannula. Epoprostenol Heliox And...if we have time. Mechanical ventilation.
CLINICAL ASSESSMENT OF THE ACUTELY UNSTABLE PATIENT Why do things go wrong in an acutely unstable patient? Evaluation of vital organ functions. Avoiding typical pitfalls.
WHY DO THINGS GO WRONG IN THE ACUTELY ILL PATIENT? Vital functions have not been evaluated. Clinical findings cannot be interpreted. Search for diagnosis supersedes the evaluation of vital functions. There is a discrepancy between working diagnosis and clinical status, its evolution goes unnoticed. Cookbook medicine obscures the importance of evaluation and support of vital functions.
POINTS TO BE CONSIDERED IN THE EVALUATION OF A POTENTIALLY UNSTABLE PATIENT. Is there dysfunction of vital organs or a high risk for vital organ dysfunction? Are there immediate therapeutic or supportive interventions needed? What is the likely etiology. Is there a specific treatment available? What is the expected clinical course? What is the immediate response to therapeutic interventions? And what is the need for further treatment? Where can the necessary treatment best be commenced in terms of available resources, logistics, and facilities?
EVALUATION OF VITAL ORGAN FUNCTIONS First question. Is there a problem? Is cardiopulmonary resuscitation needed? Evaluation of airway and breathing. Evaluation of circulation. Evaluation of the central nervous system. Dysfunction of other vital organs. Septic shock. Avoiding typical pitfalls.
IS CARDIOPULMONARY RESUSCITATION NEEDED? Unconscious, not breathing, no palpable central arterial pulse. No clear contraindication. Known living will. Documented prolonged lack of circulation. Terminal illness. Initiate CPR. Simple assessment of level of consciousness (verbal and physical stimulation) simultaneously observing and checking respiratory movements and airflow and checking the carotid pulse.
EVALUATION OF AIRWAY AND BREATHING Is the airway open, and is the patient breathing? Is the patient dyspneic? Also search for objective signs of dyspnea. Is the patient tachypneic? (or bradypneic)? Are breathing movements normal and well coordinated? Are paradoxical movements present? Does the patient reach a relaxed end-expiratory volume? Does the pulse oximetry suggest hypoxemia? Are the blood gases abnormal? Are the other vital organ functions stable (especially the cardiovascular and central nervous systems)?
CLINICAL ALARM SIGNS RESPIRATORY Tachypnea and increased inspiratory efforts. Paradoxical or uncoordinated thoracoabdominal respiratory movements. Use of auxiliary respiratory muscles. Concomitant circulatory instability. Decreased level of consciousness (preterminal symptom in respiratory failure) Hypoxemia and hypercapnia. Hypoxemia and acidosis. Hypoxemia and combined respiratory and metabolic acidosis (preterminal finding).
PROBABLE CLINICAL COURSE FOR RESPIRATORY DYSFUNCTION Expected clinical course relevant for planning treatment strategy. Rapid recovery scenarios. Intoxications and respiratory depression, after general anaesthesia, acute attack of asthma, cardiogenic acute pulmonary edema, pulmonary embolism. Prolonged recovery scenarios. Acute lung injury, ARDS, lung contusion, pneumonia induced respiratory insufficiency, unstable chest wall.
EVALUATION OF CIRCULATION. Are central pulses present? Is the cardiac output low? Is the circulation blood volume low, normal, or high? Are there symptoms and signs of insufficient tissue perfusion?
SIGNS AND SYMPTOMS OF ACUTE HYPOVOLEMIA (ORDER OF APPEARANCE) Tachycardia Reduced capillary perfusion. Reduced peripheral skin temperature (often a clearly detectable border between warm and cold skin). Decreased venous filling (first in the periphery and then centrally). Oliguria. Hypotension. Decreased level of consciousness.
CLINICAL ALARM SIGNS - CARDIOVASCULAR Hypotension. Large respiratory variations of pulse pressure. Hypotension and concomitant decreased level of consciousness.
PROBABLE CLINICAL COURSE OF CIRCULATORY DUSFUNCTION Rapid recovery scenarios. Circulatory failure due to hypovolemia, underlying cause treated. Myocardial ischemia if addressed by medicines or intervention. Even if due to pulmonary embolism if treatment commenced early and patient is responsive. Tension pneumothorax and pericardial tamponade if reversed quickly. Prolonged recovery scenarios. Pump failure secondary to prolonged ischemia, basic disease that is not rapidly reversible (myocarditis, vasculitis, acute or chronic heart failure). Septic shock.
EVALUATION OF CENTRAL NERVOUS SYSTEM Assess level of consciousness. Does the patient appear alert and are the eyes open? How big are the pupils are they symmetric and react to light? Verbal and motor response check. Is it sufficient to protect the airway? Hypoxemia, hypercapnea and hypotension can effect neuro status. Reevaluation after stabilization of circulation and gas exchange. Check hypoglycemia and pCO2 as potentially quickly reversible.
CLINICAL ALARM SIGNS - NEUROLOGICAL Acute reduction of level of consciousness. New focal neurological signs. Stiff neck. Glasgow Coma Scale of less than 9 (usually needs intubation for airway protection). Asymmetric pupils. Concern regarding intracranial pathology like bleed or large stroke.
PROBABLE CLINICAL COURSE OF ACUTE CENTRAL NERVOUS SYSTEM DYSFUNCTION Rapid recovery scenarios. Intoxications, hypoglycemia, epilepsy, mild brain injury (concussion), transient ischemia, promptly treated stroke, less severe subarachnoid hemorrhage. Prolonged recovery scenarios. Prolonged ischemia, infections, severe injuries, metabolic encephalopathies.
SEPSIS AND SEPTIC SHOCK Wide array of unspecific symptoms and signs. Often misinterpreted and often precede acute instability. Septic infection produce systemic inflammatory response syndrome. Not specific to sepsis. Symptoms Fever, tachycardia, hypotension, impaired capillary perfusion, progressing to hypovolemia, mental status changes (confusion and agitation), hyperventilation, dyspnea with hypocapnea and frequently hypoxemia
SEPSIS AND SEPTIC SHOCK - 2 Lab findings. Leukocytosis or leukopenia, thrombocytopenia, increased CRP, lactic acid, metabolic acidosis. Hypothermic, normothermic or febrile. Fundamental clinical feature. Septic patient is disproportionately sick compared to other diagnosis with similar change in vital signs. Suspect sepsis in patient with signs of cardiovascular, respiratory or mental instability.
RAPID ASSESSMENT AT BEDSIDE Get overall impression of appearance or behavior. Speak to patient. Check airflow, observe breathing movements and breath sounds, check pulses, Check control of eye opening, pupil size and reaction, and level of consciousness. Move to patients side and check breathing movements by palpation. Get an impression of the thorax and abdomen. Evaluate peripheral venous filling in upper extremities. Move to patient legs. Check pulses in femorals, check peripheral venous filling in feet, edema, Can be quickly completed in 30 -60 seconds.
NONINVASIVE VENTILATION Allows mechanical ventilation without an ET tube. Main benefits are decreases in intubation rates, mortality rate, and a number of infectious complications, particularly pneumonia. Well established in COPD exacerbations, improvement in blood gases and lung mechanics, decrease in rates of intubation, pneumonia and length of ICU and hospital stay. Also established for pulmonary edema. Controversy if better to use CPAP or PS with PEEP. Under study for hypoxemic respiratory failure, immunosuppressed hypoxemic patients, hasten vent weaning, and to avoid reintubation after unsuccessful extubation.
NIV FOR ACUTE HYPERCAPNIC RESPIRATORY FAILURE MECHANISM Respiratory failure occurs after a period of rapid shallow breathing, increasing dead space-to-tidal volume ratio with subsequent hypoventilation and respiratory acidosis. High respiratory centre stimulation together with large intrathoracic pressure swings generated by respiratory muscles are insufficient to generate adequate tidal volumes. Rapid shallow breathing facilitate an increase in pulmonary hyperinflation. This worsens muscle-length tension. All of the above contributes to increasing pCO2 and acidosis.
NIV IN HYPERCAPNIC RESPIRATORY FAILURE Increase in respiratory effort leads to respiratory pump failure and then eventually respiratory arrest. Mechanical ventilation allows rest. Pressure support allows increased tidal volume with same effort, PEEP (counters auto-PEEP) reduces patients effort to breathe and markedly modifies the breathing pattern. Increase in tidal volume and decrease in rate improves alveolar ventilation. Helps decrease the pCO2. The pH improvement in the first hours on BiPAP is a success predictor.
NIV IN CARDIOGENIC RESPIRATORY FAILURE. CPAP in cardiogenic respiratory failure improves oxygenation as it increases functional residual capacity. Favorable CPAP hemodynamic effects are decrease in RV preload, which may increase RV afterload, decreases in LV preload, decrease in LV transmural pressure, and decrease in LV afterload. With CPAP, improvement in lung compliance, significant decreases in elastic and resistive components of the work of breathing, significant reductions in the work of breathing.
INDICATIONS FOR BIPAP COPD exacerbation Acute pulmonary edema. Selected populations of acute respiratory failure Other indications Facilitation of weaning Post operative respiratory failure. DNR patients. Community acquired pneumonia. OSA and OHS patients.
CONTRAINDICATIONS FOR NIV Non-respiratory organ failure: Encephalopathy Severe GI bleeding Hemodynamic instability with or without cardiac ischemia. Facial trauma or surgery. Inability to protect airway, risk of aspiration. Patient intolerance or uncooperative patient. Claustrophobia.
TECHNIQUES, EQUIPMENT AND VENTILATOR MODES Full face masks and nasal plugs cause a greater decrease in pCO2 than nasal. Nasal masks have greater acceptance. Usually pressure support with PEEP. May use ICU ventilator. Allows patient high control of respiratory rate and timing, inspiratory flow, and tidal volume.
HIGH FLOW NASAL CANNULA O2 is typically delivered via low flow systems (nasal cannula or masks) or high flow systems (venturi masks or non-rebreathers). Do not deliver a reliable fraction of inspired O2. Poorly tolerated for prolonged periods due to inadequate warming and humidification. Newer systems reliably deliver warmed and humidified O2 at high flows through nasal cannulae.
HIGH FLOW O2 NASAL CANNULA Small pliable prongs. Improved comfort. Warming and humidification of secretions. Facilitates secretion removal, prevent desiccation and epithelial injury. Washout of nasopharyngeal dead space. Improved washout allows a higher fraction of minute ventilation to participate in alveolar gas exchange. Continuous positive airway pressure. Buildup of pressure, peak at end expiration. PEEP effect. Every 10L/min yields 0.7 or 0.35 cm H20 airway pressure. High flow rates. Minimal entrainment of room air, more accurate O2 delivery.
HIGH FLOW NASAL CANNULA Parameters needing to be set. FiO2 and Flow rate. Indications. Not absolute. Tried in various settings. Observational studies. No definite benefit. Still used in place of other high flow O2 systems, better tolerated. In place of NIV, but unlikely to provide sufficient PEEP in moderate to severe ARDS or adequate ventilation in patients with hypoventilation. May reduce work of breathing less than NIV.
HIGH FLOW NASAL CANNULA Medical patients with severe hypoxemic respiratory failure. Improved oxygenation, lower respiratory rate. Decreased MV and comfort. Tidal volume unchanged. End-expiratory lung volume and dynamic lung compliance increased. No consistent or convincing benefit in outcomes. Post extubation support. Post operative respiratory failure. Intubation support.
HIGH FLOW NASAL CANNULA - CONTRAINDICATIONS Abnormalities or surgery of the face, nose, or airway that preclude an appropriate-fitting nasal cannula. Venous thrombosis. Theoretical. Related to high pressure. Abdominal distension, aspiration, barotrauma (rare, pneumothorax). Recognition of ARDS may be impacted due to improved p/f ratio. Delay in intubation.
PULMONARY HYPERTENSION AND POOR OXYGENATION. Epoprostenol. (Flolan, Veletri). Strong vasodilator of all vascular beds. Potent endogenous inhibitor of platelet aggregation. The reduction in platelet aggregation results from epoprostenol's activation of intracellular adenylate cyclase and the resultant increase in cyclic adenosine monophosphate concentrations within the platelets. Additionally, it is capable of decreasing thrombogenesis and platelet clumping in the lungs by inhibiting platelet aggregation.
VASCULAR ENDOTHELIUM DILATATION Hypoxia secondary to ARDS (off-label use): Inhalation (off-label): Initial: 0.01 to 0.05 mcg/kg/minute; increase dose in stepwise fashion based on efficacy and tolerability. Wean by reducing dose by 0.01 mcg/kg/minute every 1 to 2 hours as tolerated. Also used in pulmonary hypertension. No dosage adjustment for renal or liver abnorm.
HELIOX Inert, non-toxic gas. Lighter than nitrogen and oxygen. Does not enable laminar airflow, it can reduce the airflow resistance of turbulent flow, as resistance is proportional to the density of the mixture. Potential use in a variety of disease processes characterized by airflow limitation. Optimal helium-oxygen ratio is not known. 80:20/70:30 Mechanical ventilators have to be recalibrated.
Next Section. Do we really want to?
MODES OF MECHANICAL VENTILATION Pressure versus volume ventilation. Volume targeting. Specific tidal volume is set, flow waveform, and peak flow. Focus is on ensuring MV is maintained at target level. Pressure targeting. Targeted peak airway (= peak alveolar pressure) is set and sometimes inspiratory time. Tidal volume and gas flow are allowed to vary breath to breath. Focus on ensuring targeted alveolar pressure is met but never exceeded.
RANGE OF VENTILATOR MODES Classic modes Assist/control, assist(pressure support) and synchronized intermittent mandatory ventilation. Available for more than 20 yrs. New modes Designed to improve patient-ventilator synchrony Most based on pressure ventilation format. Most can be classified as modes that adjust gas delivery within a given breath. Computerized control of gas delivery.
CONTROL MODE Original mode Controls all aspect of gas delivery. Assumes a passive recipient of mechanical ventilation. Nowadays achieved by sedation to apnea in OR by anaesthesia. Controlled ventilation is available in both pressure and ventilation formats.
ASSIST / CONTROL MODE Essentially control mode with sensitivity set to allow easy patient triggering of a breath. Patient determines respiratory rate. Back up to ensure minimum level of ventilation. Most commonly used mode. Set parameters FiO2, back up rate, sensitivity and PEEP . Pressure ventilation. Target airway pressure, insp time. Volume ventilation. Tidal volume, flow waveform, peak flow and inspiratory time.
PRESSURE SUPPORT Allows patient greater control over the process. Patient triggers a breath and ending is also based on patient demand. Only gas delivery set is pressure level and sensitivity. Back up rate is available.
SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION Advocates commend benefits of spontaneous breathing between breaths. However, work of breathing can be excessive. Respiratory centre has difficulty rapidly changing outputs based on ventilatory mode. May increase patient-ventilator synchrony.
PRESSURE-REGULATED VOLUME CONTROL Targets both a maximum airway pressure and tidal volume. Variation of pressure assist / control. Deliver a test breath at low pressure. Measures volume. Calculated pressure to deliver targeted tidal volume. On every subsequent breath, tidal volume delivered is reassessed. Pressure is adjusted 0 1 cmH2O. Concern. In patients with a strong drive, and added stimulus of hypoxemia, fevers, sepsis, etc, patient may get little to no support inappropriately.
VOLUME SUPPORT Operates essentially same as PRVC. Based on pressure support not pressure assist / control . Same assessment breath to breath to assess pressure needed to deliver targeted tidal volume. Same concern regarding too strong a drive. Exactly same as setting up pressure support ventilation with addition of a volume target and maximum pressure.
ADAPTIVE SUPPORT VENTILATION Very unique mode. Operates on pressure ventilation format. Adjusts ventilator setting for an 'ideal' ventilatory pattern. Requiring least amount of patient and ventilator work. Goal is to provide preset level of minute ventilation while minimizing the total work of breathing. Provide patients IBW. And % of minimal MV to be delivered, between 25% to 350%.
AUTOMATIC TUBE COMPENSATION Sometimes called electronic extubation. Resistance properties of all sizes of ET and trach in memory and continually measuring gas flow. Goal is to provide sufficient support during inspiration and decompression during exhalation to maintain tracheal pressure equal to baseline. Designed only to offload flow resistive properties of the artificial airway.
PROPORTIONAL ASSIST VENTILATION Similar to ATC. Mechanics of total respiratory system. Pressure assist in proportion to patient desired tidal volume and instantaneous inspired flow. Automatically adjusted to meet patient demand. Only useful in patients with stable respiratory drives. And an acceptable respiratory pattern.
VOLUME ASSURED PRESSURE SUPPORT Also referred to as pressure augmentation. Combine initial high flow of a pressure limited breath with constant volume delivery of a volume targeted breath. Differs from PRVC and volume support as it maintains ventilatory support independent of patient demand.