Rare Diseases of the Hypothalamus and Pituitary
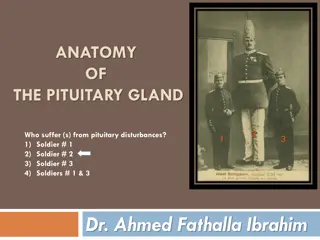
Diseases of the hypothalamus and pituitary are rare, with an annual incidence of approximately 1:50,000. Investigation and treatment involve multiple glands due to the pituitary's central role in endocrine axes. Explore how to investigate patients with suspected pituitary hypothalamic disease, identify hormonal deficiencies, hormone excess, and establish anatomy and diagnosis through imaging tests.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
THE HYPOTHALAMUS &THE PITUITARY GLAND
Diseases of the hypothalamus and pituitary are rare, with an annual incidence of approximately 1:50 000. The pituitary plays a central role in several major endocrine axes, so that investigation and treatment invariably involve several other glands
How to investigate patients with suspected pituitary hypothalamic disease Identify pituitary hormone deficiency ACTH deficiency Short ACTH stimulation test (see Box 20.46, p. 776) Insulin tolerance test (see Box 20.59, p. 786): only if uncertainty in interpretation of short ACTH stimulation test (e.g. acute presentation) LH/FSH deficiency In the male, measure random serum testosterone, LH and FSH In the pre-menopausal female, ask if menses are regular In the post-menopausal female, measure random serum LH and FSH (which would normally be > 30 mU/L) TSH deficiency Measure random serum T4 Note that TSH is often detectable in secondary hypothyroidism, due to inactive TSH isoforms in the blood
How to investigate patients with suspected pituitary hypothalamic disease Identify pituitary hormone deficiency Growth hormone deficiency Only investigate if growth hormone replacement therapy is being contemplated Measure immediately after exercise Consider other stimulatory tests Cranial diabetes insipidus Only investigate if patient complains of polyuria/polydipsia, which may be masked by ACTH or TSH deficiency Exclude other causes of polyuria with blood glucose, potassium and calcium measurements Water deprivation test or 5% saline infusion test
How to investigate patients with suspected pituitary hypothalamic disease Identify hormone excess Measure random serum prolactin Investigate for acromegaly (glucose tolerance test) or Cushing s syndrome if there are clinical features
How to investigate patients with suspected pituitary hypothalamic disease Establish the anatomy & diagnosis Consider visual field testing Image the pituitary and hypothalamus by MRI or CT
Hypopituitarism Hypopituitarism describes combined deficiency of any of the anterior pituitary hormones. The clinical presentation is variable and depends on the underlying lesion and the pattern of resulting hormone deficiency. The most common cause is a pituitary macroadenoma
Clinical assessment The presentation is highly variable. With progressive lesions of the pituitary there is a characteristic sequence of loss of pituitary hormone secretion. Growth hormone secretion is often the earliest to be lost. In adults, this produces lethargy, muscle weakness and increased fat mass, but these features are not obvious in isolation. Next, gonadotrophin (LH and FSH) secretion becomes impaired with, in the male, loss of libido and, in the female, oligomenorrhoea or amenorrhoea. Later, in the male there may be gynaecomastia and decreased frequency of shaving. In both sexes axillary and pubic hair eventually become sparse or even absent and the skin becomes characteristically finer and wrinkled. Chronic anaemia may also occur. The next hormone to be lost is usually ACTH, resulting in symptoms of cortisol insufficiency.
In contrast to primary adrenal insufficiency (p. 774), angiotensin II-dependent zona glomerulosa function is not lost and hence aldosterone secretion maintains normal plasma potassium. However, there may be postural hypotension and a dilutional hyponatraemia for three reasons: Failure of vasoconstriction in the absence of cortisol results in pooling of blood in the legs on standing. Antidiuretic hormone (ADH) release is enhanced by hypotension and cortisol deficiency. Cortisol is required for normal water excretion by the kidney.
In contrast to the pigmentation of Addisons disease, a striking degree of pallor is usually present, principally because of lack of stimulation of melanocytes by - lipotrophic hormone ( -LPH, a fragment of the ACTH precursor peptide) in the skin. Finally, TSH secretion is lost with consequent secondary hypothyroidism. This contributes further to apathy and cold intolerance. In contrast to primary hypothyroidism, frank myxoedema is rare, presumably because the thyroid retains some autonomous function.
The onset of all of the above symptoms is notoriously insidious. However, patients sometimes present acutely unwell with glucocorticoid deficiency. This may be precipitated by a mild infection or injury, or may occur secondary to pituitary apoplexy. Other features of pituitary disease may be present
Investigations Tests of growth hormone secretion GH levels are commonly undetectable, so a choice from the range of stimulation tests is required*: 1 hour after going to sleep Frequent sampling during sleep Post-exercise Insulin-induced hypoglycaemia Arginine (may be combined with GHRH) Glucagon Clonidine
Investigations Pituitary dynamic tests All patients with biochemical evidence of pituitary hormone deficiency should have an MRI or CT scan to identify pituitary or hypothalamic tumours. If a tumor is not identified, then further investigations are indicated to exclude infectious or infiltrative causes.
Management Treatment of acutely ill patients is similar to that described for adrenocortical insufficiency, except that sodium depletion is not an important component to correct. Once the cause of hypopituitarism s established, specific treatment of a pituitary macroadenoma, for example may be required.
Cortisol replacement Hydrocortisone should be given if there is ACTH deficiency. Mineralocorticoid replacement is not required.
Thyroid hormone replacement Thyroxine 100 150 g once daily should be given Unlike in primary hypothyroidism, measuring TSH is not helpful in adjusting the replacement dose because patients with hypopituitarism often secrete glycoproteins which are measured in the TSH assays but are not bioactive. The aim is to maintain serum T4 in the upper part of the reference range. It is dangerous to give thyroid replacement to patients with adrenal insufficiency without first giving glucocorticoid therapy, since this may precipitate adrenal crisis.
Sex hormone replacement This is indicated if there is gonadotrophin deficiency in men of any age and in women under the age of 50 to restore normal sexual function and to prevent osteoporosis
Growth hormone replacement Growth hormone (GH) is administered by daily subcutaneous self-injection to children and adolescents with GH deficiency and, until recently, was discontinued once the epiphyses had fused. However, although hypopituitary adults receiving full replacement with hydrocortisone, thyroxine and sex steroids are usually much improved by these therapies, some individuals remain lethargic and unwell compared with a healthy population.
Pituitary tumour Pituitary tumours produce a variety of mass effects, depending on their size and location, but also present as incidental findings on CT or MRI, or with hypopituitarism,as described above. A wide variety of disorders can present as mass lesions in or around the pituitary gland Most intrasellar tumours are pituitary macroadenomas (most commonly non-functioning adenomas, whereas the majority of suprasellar masses are craniopharyngiomas The most common cause of a parasellar mass is a meningioma
A common but non-specific presentation is with headache, which may be the consequence of stretching of the diaphragma sellae. Compression of the neural connections between the retina and occipital cortex may lead to a visual field defect. Although the classical abnormalities associated with compression of the optic chiasm are bitemporal hemianopia (see Fig. 20.29) or upper quadrantanopia, any type of visual field defect can result from suprasellar extension of a tumour because it may compress the optic nerve (unilateral loss of acuity or scotoma) or the optic tract (homonymous hemianopia). Optic atrophy may be apparent on ophthalmoscopy. Lateral extension of a sellar mass into the cavernous sinus with subsequent compression of the 3rd, 4th or 6th cranial nerves may cause diplopia and strabismus.
Occasionally, pituitary tumours infarct or there is bleeding into cystic lesions. This is termed pituitary apoplexy and may result in sudden expansion with local compression symptoms and acute-onset hypopituitarism. Non-haemorrhagic infarction can also occur in a normal pituitary gland; predisposing factors include obstetric haemorrhage (Sheehan s syndrome), diabetes mellitus and raised intracranial pressure.
Investigations Patients suspected of having a pituitary tumour should undergo MRI or CT. Whilst some lesions have distinctive neuroradiological features, definitive diagnosis often requires biopsy which is usually done at the same time as operative treatment to resect or debulk a tumour that is compressing the optic chiasm. All patients with (para-) sellar space-occupying lesions should have pituitary function assessed.
 undefined
undefined