Quality of End-of-Life Care for Vietnam-Era Veterans: A Retrospective Analysis
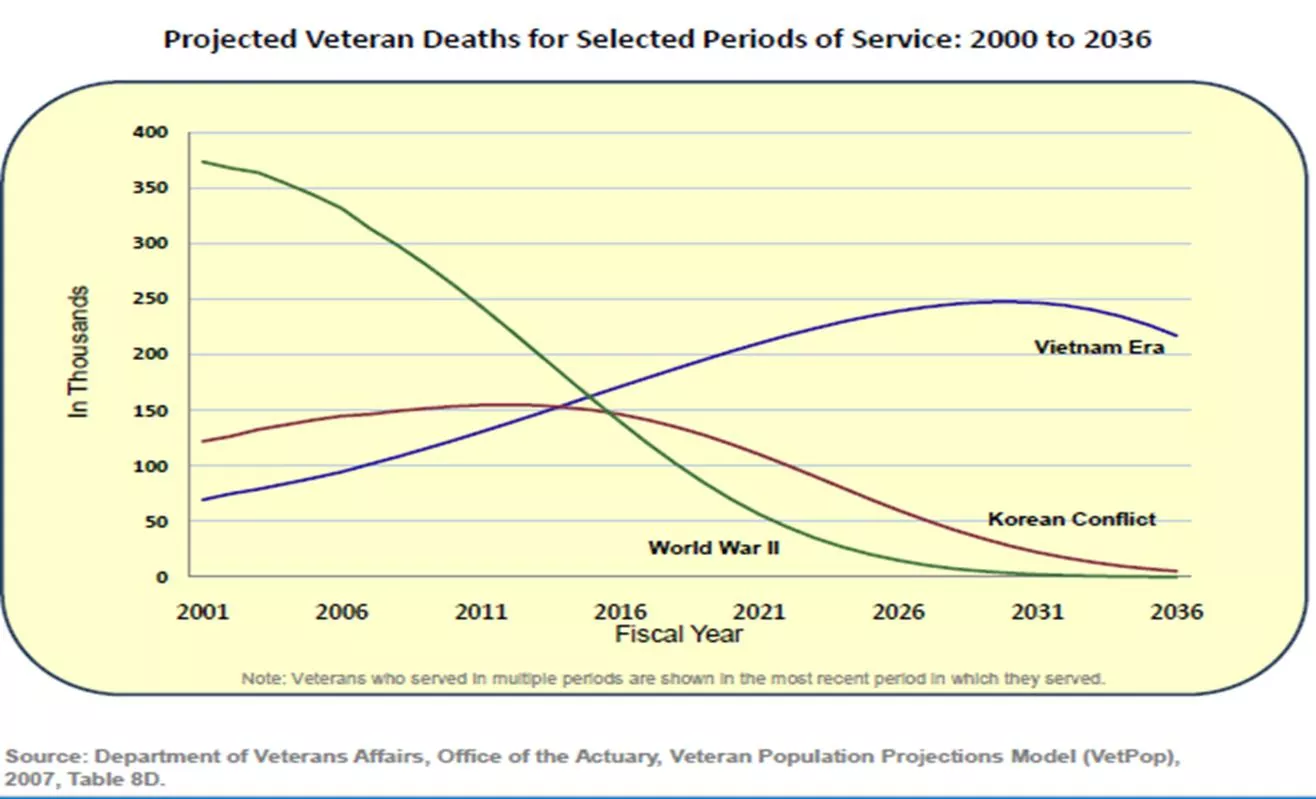
This study examines the quality of end-of-life care for Vietnam-era veterans compared to veterans of prior war eras. Data analysis includes clinical characteristics, healthcare utilization, and quality indicators from bereaved family members of deceased veterans. The research highlights the unique care needs of Vietnam-era veterans at the end of their lives and aims to improve the quality of care provided to this specific group of veterans.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
QUALITY OF END-OF-LIFE CARE FOR VIETNAM-ERA VETERANS Ann Kutney-Lee, PhD, RN, FAAN & Shimrit Keddem, PhD, MPH National Hospice & Palliative Care Webinar January 23, 2020
Objectives 1) Describe clinical characteristics, healthcare utilization and quality indicators among Vietnam-era Veterans at end-of-life. 2) Compare the clinical characteristics, healthcare utilization and quality indicators of Vietnam-era Veterans at end-of-life with Veterans of prior war eras. 3) Identify the unique care needs of Vietnam-era Veterans at end-of- life as described by bereaved family members.
Quantitative Design Retrospective, cross-sectional analysis Linked data sources from October 2012- September 2017 Bereaved Family Survey (BFS) collected from family members of deceased Veterans Corporate Data Warehouse (CDW) for clinical characteristics, utilization and quality indicators The final sample included inpatient deaths among Vietnam and World War II/Korean War-era Veterans (n=87,526) and associated BFS responses from family members(n=39,296)
Selected Demographic Characteristics Characteristic Vietnam War-Era (n=45,860) World War II- Post-Korean War-Eras (n=41,666) Age, mean (SD)* 68.8 (6.5) 85.5 (6.0) Race/Ethnicity, % Non-Hispanic white * 69.5 72.1 Non-Hispanic black * 19.0 13.2 Hispanic * 4.8 8.1 Other/did not disclose 6.4 6.3 Next of Kin, % Spouse * 37.9 35.1 Child * 27.2 46.1 Sibling * 18.6 5.2 Other family 7.3 7.2 Other non-family * 8.7 6.2 Notes: *p<0.001. Percentages may not add to 100 due to rounding.
Selected Clinical Characteristics Characteristic Vietnam War-Era (n=45,860) World War II- Post-Korean War-Eras (n=41,666) Any service-connection, % 54.4 36.4 100% service-connected, % 23.4 8.2 Veteran Priority Status, % High Disability 44.9 34.2 Exposed to Agent Orange, % 21.7 <0.1 Comorbid conditions, mean (SD) 8.5 (3.3) 7.5 (3.2) Notes: All differences significant at p<0.001.
Most Common Mental Health/ Substance Abuse Conditions Condition Vietnam War-Era (n=45,860) World War II- Post-Korean War-Eras (n=41,666) Depression, % 33.0 23.5 Anxiety, % 18.4 13.5 Alcohol abuse, % 24.0 5.7 Post-traumatic stress disorder (PTSD), % 16.5 5.7 Other mental health disorders, % 10.8 9.2 Drug abuse, % 11.8 2.0 Notes: All differences significant at p<0.001.
Selected Utilization/Process Measures, Age-Adjusted Measure Vietnam War-Era (n=45,860) World War II- Post-Korean War-Eras (n=41,666) Estimated Difference Outpatient visits in last year of life, mean (SD) 55.8 (0.2) 50.4 (0.2) 5.4 *** Days in hospital in last year of life, mean (SD) 72.3 (0.5) 53.2 (0.6) 19.1 *** Palliative Consult, % 70.4 72.0 -1.6 ** Venue of death, % Acute care unit 20.4 23.3 -2.8 *** CLC 18.1 15.8 2.1 *** Chaplain contact, % 84.3 84.6 <0.1 Notes: **p<0.01 ***p<0.001.
Adjusted BFS Item Scores by War Era, FY2013-2017 Note: Estimates adjust for age and BFS nonresponse. For purposes of consistency and presentation with the BFS-PM and interpretation of scores, the three factor scores were standardized to a 0-100 scale.
Qualitative Data We reviewed 2,784 open-ended response from the BFS Data were from 2013-2017, all facilities Responses to the following questions: 1) Is there anything else that you would like to share about the Veteran s care during his last month of life? 2) Is there anything else that you would like to share about how the care could have been improved for the Veteran?
Qualitative Methods Applied thematic analysis using qualitative data analysis software Identified successes and challenges in the bereavement experience of family members Only substantive responses were include (e.g. Thank you! was removed) Four evaluators reviewed the data and applied a series of codes to sort the data We compared Vietnam vs pre-Vietnam era families responses to look for differences.
Patient attentiveness related to food/nutrition provision Good patient hygiene Good pain management Clean, welcoming environment Housing/space accomodations Pet visitation Activities of Daily Living (ADL allowances Clear & open communication on health status Care team on same page Staff availability to family in person & by phone Efficient benefits & paperwork assistance Spiritual & emotional support Timely funeral support Support Comfort Honor Validation Patient & family complaints heard & addressed efficiently Patient & identified family listened to as active partners in decision making Family informed & kept up to date on patient health changes Staff & phone responsiveness Patient advocacy Compassion, empathy, & kindness Dignity & respect during illness Dignity & respect upon passing Relationship building & treating patient like family Respect of personal property Respect of privacy
Support - Positive The physician was excellent! He communicated with us every day, updating us on his condition and helping us to make difficult end of life decisions. Pre-Vietnam The buzzer was always answered when I called for help! The doctors were always willing to do whatever they had to do to make my husband comfortable. Everyone who touched my husband s life was wonderful! I give [the] Unit an A+ for the care that we received. Vietnam
Support - Negative "The biggest issue in my opinion was that there were too many people (doctors) that were involved in taking care of him. I would ask a question of one individual and given an answer. One hour later, ask a question and given a totally different answer by someone else. Vietnam I had (have) the impression the hospice unit is short on the number of hospice trained nurses they have on duty and so some staff is overworked, too many back-to-back shifts, too many nurses borrowed from elsewhere. Pre-Vietnam
Comfort - Positive However, when it became time for hospice, we both knew that the hospice unit at the VA was where we wanted to be. The staff were so knowledgeable, kind, and supportive. They made sure he was comfortable and pain-free, which meant everything to us. Vietnam I would like to mention the dietician who came up to my dad s room to talk about what he could eat that would make it easier for him. Pre-Vietnam
Comfort - Negative When he received his terminal diagnosis, it took way too long for him to be seen by the palliative care doctor and to be adequately managed for pain. Finally, his pain was managed but his emotional distress was not. Pre-Vietnam During the last week before his death, they were serving his hard food that [the patient] couldn t eat. They should have given him more mashed potatoes & gravy, cottage cheese, soup, V-8, etc. Pre- Vietnam
Honor - Positive They took care of my father as though he was theirs. Staff brought him food from home and local restaurants, kissed and hugged him every chance they got. They treated him with respect and love. I am eternally grateful. Pre-Vietnam We were so touched when they covered [his] body with the flag and the staff and any patient able to stand at attention.The hall played taps as his body was rolled out. I appreciated the honor given to veterans. The ceremony meant so much to us. Pre-Vietnam
Honor - Negative After he passed away, I was at the bedside and the male bedside caregiver, nurse kept entering the room asking me how much longer? (I was emotionally upset of his sudden passing) This male bedside caregiver nurse was rude and should of never said this to me, it made me feel rushed and that he did not care. Vietnam At one point a social worker was talking about what would be done with his body (moved to the cooler) after he died. I was at his bedside he was conscious, and I felt she should not have discussed that subject in his room. She could have asked me to step outside or waited for another appropriate time. Pre-Vietnam
Validation - Positive But when I could not be there I would call and talk to one of his nurses and get an update on him. I also would send him text messages, which he could not pull up and they would go in and pull them up on his phone and read them to him and then call me and tell me they had read them. Pre-Vietnam The nurses were very helpful & arranged a computer so [Name of Patient] could watch our daughters college graduation on streaming video. Vietnam
Validation - Negative I was not kept informed about what they were doing for my dad or why. My asking seemed to annoy some of the nurses. Pre-Vietnam We were promised that we would be informed when my brother was near the end so that we could be with him. However, that did not happen, and he was deceased when we arrived at the hospital. We felt terrible about it. - Vietnam
Agent Orange He had Alzheimer s & I say related to Agent Orange, but I could not find anyone to support me. Vietnam I would like to express that the care my husband received throughout the VA healthcare in (both) [Name of VA Hospital 1] and in [Name of VA Hospital 2] was very good. Not only in his final months, but for all the years of his many illnesses he had due to battling Agent Orange. It was good. He had the best doctors and nurses for his care. He was always treated with the utmost dignity and honor as the soldier he was. Vietnam
Support - Recommendations Have readily available care teams who answer questions and provide honest expectations and guidance Have readily available staff who provide administrative, benefits and end of life (EOL) support Provide clear communication that is upfront, honest, and personalized. Provide a main point of contact to help navigate the VA care system, assist with benefits, and answer any questions. Provide treatment options and more education on the dying process. Improve the efficiency of benefit and funeral provision.
Comfort - Recommendations Have readily available care teams who are attentive to a patient s needs Provide fresh, high quality food for all patients Promptly adjust to the patient s changing health needs Provide private rooms whenever possible Provide housing and travel reimbursement support Accommodate activities of daily living when possible
Honor - Recommendations Have readily available care teams who communicate routinely, respectfully and compassionately. Have readily available staff who maintain the patient and family s dignity and honor Ensure staff are trained to provide empathy, compassion, and professionalism. Prevent and address loss of personal property in a timely and respectful manner.
Validation - Recommendations Have readily available staff who advocate for the patient s changing needs. Have readily available staff who are responsive to the family s needs Keep family up to date on the progress and status of the patient Provide an up-to-date patient portal for family members Establish an identification system so family members can call to receive health information over the phone. Provide Wi-Fi to access Skype for long-distance family members Simplify the phone system and leave extension information when calling back. Act upon complaints efficiently.
Conclusion VA s current practices and programs are largely meeting the needs of Vietnam Veterans and their families; however, Vietnam-era Veterans demonstrate some unique clinical characteristics from prior generations that should be considered when planning EOL care, including mental health (specifically PTSD), disabilities, and Agent Orange-related conditions.