Overview of the Circulatory System and the Heart
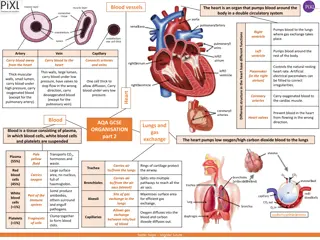
The circulatory system comprises the cardiovascular system and the lymphatic system. The heart, a four-chambered double pump, plays a crucial role in pumping blood through the vessels to the lungs and body cells. The heart's structure, function, and components like the atria, ventricles, and valves are essential in understanding its role in circulation.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Lecture 1 Dr. Shaimaa Munther
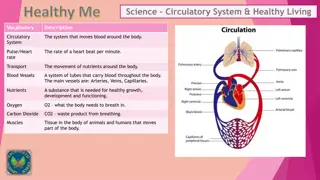
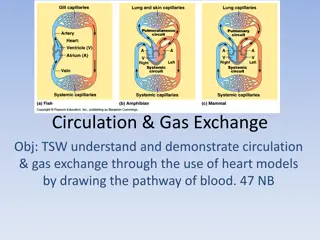
circulatory system The consists of two subdivisions: The cardiovascular system and the lymphatic system. The cardiovascular system consists of the heart and blood vessels, and the lymphatic system, which lymphatic lymphoid tissues within the spleen, thymus, tonsils, and lymph nodes. includes vessels and
The heart is a four-chambered double pump. Its pumping action creates the pressure needed to push blood through the vessels to the lungs and body cells. At rest, the heart of an adult, pumps about 5 liters of blood per minute. At this rate, it takes about 1 minute for blood to be circulated to the most distal extremity and back to the heart.
Heart is about the size of a fist, the hollow, cone-shaped heart is divided into four chambers. The right and left atria receive blood from the venous system; the right and left ventricles pump blood into the arterial system. The right atrium and ventricle are separated from the left atrium and ventricle by a muscular wall, or septum. This septum normally prevents mixture of the blood from the two sides of the heart Between the atria and ventricles, there is a layer of dense connective tissue known as the fibrous skeleton of the heart . The right ventricle pumps blood to the lungs, where the blood becomes oxygenated; The left ventricle pumps oxygenated blood to the entire body.
Myocardium : Bundles of myocardial cells in the atria attach to the upper margin of this fibrous skeleton and form a single functioning unit. Special conducting tissue is needed to carry action potentials from the atria to the ventricles
The atria and ventricles are separated into two functional units by a sheet of connective tissue the fibrous skeleton previously mentioned. Embedded within this sheet of tissue are one-way atrioventricular (AV) valves. The AV valve located between the right atrium and right ventricle has three flaps, and is therefore called the tricuspid valve. The AV valve between the left atrium and left ventricle has two flaps and is thus called the bicuspid valve, or, alternatively, the mitral valve
The AV valves allow blood to flow from the atria to the ventricles, but they normally prevent the backflow of blood into the atria. Opening and closing of these valves occur as a result of pressure differences between the atria and ventricles When the ventricles are relaxed, the venous return of blood to the atria causes the pressure in the atria to exceed that in the ventricles. The AV valves therefore open, allowing blood to enter the ventricles. As the ventricles contract, the intraventricular pressure rises above the pressure in the atria and pushes the AV valves closed.
One-way semilunar valves : Are located at the origin of the pulmonary artery and aorta. These valves open during ventricular contraction, allowing blood to enter the pulmonary and systemic circulations. During ventricular relaxation, when the pressure in the arteries is greater than the pressure in the ventricles, the semilunar valves snap shut thus preventing the backflow of blood into the ventricles .
Like skeletal muscle cells, cardiac (heart) muscle cells, or myocardial cells, are striated; the myocardial cells are short, branched, and interconnected. Each myocardial cell is tubular in structure and joined to adjacent myocardial cells by electrical synapses, or gap junctions . The gap junctions are concentrated at the ends of each myocardial cell , which permits electrical impulses to be conducted primarily along the long axis from cell to cell. while skeletal muscle requires nervous stimulation to contract, cardiac muscle can produce impulses and contract spontaneously.
Cardiac muscle are involuntary effectors regulated by autonomic motor neurons. Action potentials that originate at any point in a mass of myocardial cells, called a myocardium, can spread to all cells in the mass that are joined by gap junctions. Behaves as a single functional unit. Thus, a myocardium contracts to its full extent each time because all of its cells contribute to that contraction.
1. Syncytium. 2. Automaticity and Rhythmicity. 3. Excitability and Conductivity. 4. Contractility.
The myocardium contracts as if it is a single Functional unit. Adjacent myocardial cells are joined end to end at structures called intercalated discs, where the Gap junctions allow ions to flow from one cell directly into the next cell making the action potentials to move with ease from one cardiac myocyte (cell A)) to stimulate the neighbor myocyte (cell B, C,...)
Conduction of Action Potentials within the heart Conduction of Action Potentials within the heart
Automaticity: The ability of the heart to initiate its own contraction independent of external stimuli. i. e., Automatic generation of cardiac impulse (the property of self- excitation). Rhythmicity: The regular generation of action potentials (cardiac impulse). i.e., the heart can beat regularly.
Normally Cardiac action potential originate in a specialized group of cells called the pacemaker. However, the rate of this spontaneous depolarization and thus the rate of the heartbeat , are regulated by autonomic innervation. If the heart of a frog is removed from the body and all neural innervations are severed, it will still continue to beat as long as the myocardial cells remain alive. The automatic nature of the heartbeat is referred to as automaticity. As a result of experiments with isolated myocardial cells and of observations, scientists have learned that there are three regions that can spontaneously generate action potentials and thereby function as pacemakers, (The SA node , the AV node and Purkinje fibers )
In the normal heart, only one of these, the sinoatrial node (SA node), functions as the primary pacemaker. The SA node is located in the right atrium near the opening of the superior vena cava, and serves as the primary (normal pacemaker of the heart. The two secondary pacemaker regions the AV node and Purkinje fibers (parts of conducting system of the myocardium) potential are suppressed by action potentials originating in the SA node
Initiation of Cardiac Electrical Activity Pacemaker cells Conduction system: - Sino-atrial (SA) node. - Atrio-ventricular (AV) node. - Bundle of His. - Purkinje system.
SA node Pacemaker potential Pacemaker potential AV node Purkinje cells Pacemaker cells can spontaneously and regularly initiate action potential
SA node is the normal primary pacemaker of the heart (fastest rate; 100-110 times per minute). The AV node is a secondary pacemaker (40 to 60 /minute). The Purkinje system is a tertiary pacemaker (15 and 40).
Although the SA node discharges at an intrinsic rhythmical rate of 100-110 times per minute but the pulse rate averages 70 or 80 times per minute, this is because of the effect of vagal tone.
SA node does not have a stable resting potential which starts at about 60 mV. membrane This is due to the inherent leakiness of the SA nodal fibers to Na+ influx). rising the membrane potential up to a threshed to fire an action potential. ions (Na+
Factors that affect the rate of discharge of SA node: Factors affecting heart rate : Autonomic nerves activity Autonomic nerves activity: Sympathetic activity Sympathetic activity Tachycardia Positive chronotropy generation of c- -AMP generation of c AMP Norepinephrine Norepinephrine 1 1- -adrenoreceptors adrenoreceptors increases the slope of phase 4 increases the slope of phase 4 Channels opening Channels opening ion influx ion influx
The cardiac impulse will not travel from the atria into ventricles too rapidly (why and how). There transmission of the cardiac impulse in the AV node (0.12 sec) to allow time for the atria to empty their blood into the ventricles before ventricular contraction begins. is a delay of
Q / As previously mentioned, two other regions in the heart, the AV node and Purkinje fibers, can potentially serve as pacemakers but are normally suppressed by action potentials originating in the SA node. A/ This is because their rate of spontaneous depolarization is slower than that of the SA node. Thus, the potential pacemaker cells are stimulated by action potentials from the SA node before they can stimulate themselves through their own pacemaker potentials. If action potentials from the SA node are prevented from reaching these areas (through blockage of conduction), they will generate pacemaker potentials at their own rate and serve as sites for the origin of action potentials; they will function as pacemakers. A pacemaker other than the SA node is called an ectopic pacemaker, or alternatively, an ectopic focus. So, the rhythm set by such an ectopic pacemaker is usually slower than that normally set by the SA node.
During the period of diastole, the SA node exhibits a slow spontaneous depolarization called the pacemaker potential, spreads from myocardial cell to myocardial cell through the gap junctions that connect them and spread from the through the atria, and, by means of conducting tissue, into the ventricles.
Once myocardial cell has been stimulated by action potentials originating in the SA node, it produces its own action potentials. Resting membrane potential : The majority of myocardial cells have potentials of about ( 85 mV) . resting membrane Depolarization phase : When stimulated by action potentials from a pacemaker region, these cells become depolarized to threshold, at which point their voltage-regulated Na + gates open leading to upshoot phase of the action potential due to the rapid inward diffusion of Na + through fast Na + channels. Following the rapid reversal of the membrane polarity, the membrane potential quickly declines to about 15 mV. Unlike the action potential of other cells, however, this level of depolarization is maintained for 200 to 300 msec before repolarization.
Plateau phase results from a slow inward diffusion of Ca 2 + through slow Ca 2 + channels, which balances a slow outward diffusion of K + . Rapid repolarization phase : at the end of the plateau phase is achieved, as in other cells, by the opening of voltage-gated K + channels and the rapid outward diffusion of K+ brings the action potential phase toward the end . NOTE/ The long plateau phase of the myocardial action potential distinguishes it from the spike-like action potentials in axons and muscle fibers. The plateau phase is accompanied by the entry of Ca 2+ , which begins excitation-contraction coupling as described shortly .
The mechanism of excitation-contraction coupling in myocardial cells, involving Ca 2 + - stimulated Ca 2 + release . In summary: 1. The depolarization of action potentials, conducted along the sarcolemma and transverse tubules, briefly opens voltage-gated Ca 2 + channels in the plasma membrane , allows some Ca 2 + to diffuse into the cytoplasm from the extracellular fluid, 2. This extracellular Ca 2 + stimulates the opening of Ca 2 + release channels in the sarcoplasmic reticulum, which had previously stored 3. Ca 2 + diffuses out of the sarcoplasmic reticulum, binds to troponin, and stimulates contraction. 4. During the repolarization phase of the action potential, the concentration of Ca 2 + within the cytoplasm is lowered & Ca 2 + removed back into the sarcoplasmic reticulum by a Ca 2 + ATPase pump, and the remaining Ca2+ out of the cytoplasm thereby allowing the myocardium to relax during repolarization .
Phase 0 (upstroke): initial rapid depolarization (Na+ influx). Phase 1 (partial repolarization): K+efflux (K+ outflow) Phase 2 (plateau): prolonged plateau is due to slower and prolonged opening voltage-gated Ca+2channels with Ca+2influx. Phase 3 (rapid repolarization): by (K+efflux). Phase 4 repolarization): by Na+-K+pump. of the (complete
Muscle action potential Skeletal muscle contraction
Absolute refractory period (ARP): it is the interval during which no action potential can be produced, regardless of the stimulus intensity. It lasts the upstroke plus plateau and initial repolarization repolarization at about -50 to -60 mV. This period prevents waves summation and tetanus. till mid- Relative refractory period (RRP): it is the interval during which a second action potential can be produced but at higher stimulus intensity. It lasts from the end of ARP (midrepolarization) and ends shortly before repolarization complete
Action potentials that originate in the SA node spread to adjacent myocardial cells of the right and left atria through the gap junctions between these cells. Because the myocardium of the atria is separated from the myocardium of the ventricles by the fibrous skeleton of the heart, however, the impulse cannot be conducted directly from the atria to the ventricles . Specialized conducting tissue, composed of modified myocardial cells, is thus required. These specialized myocardial cells form the AV node, bundle of His, and Purkinje fibers. Once the impulse has spread through the atria, it passes to the atrioventricular node (AV node), which is located on the inferior portion of the interatrial septum. From here the impulse continues through the atrioventricular bundle , or bundle of His .Within the myocardium of the ventricles, the action potential spreads from the inner (endocardium) to the outer (epicardium) side This causes both ventricles to contract simultaneously and eject blood into the pulmonary and systemic circulations