Overview of Pelvic Inflammatory Diseases (PID) in Women
Pelvic Inflammatory Diseases (PID) refer to infections in the upper female genital tract, including the uterus, Fallopian tubes, and ovaries. Learn about symptoms, risk factors, and complications of PID.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
PELVIC INFLAMMATORY DISEASES (PID) By: Ass. Prof.Dr.Inaam Faisal
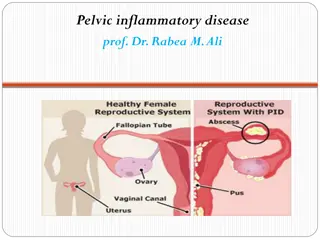
Pelvic inflammatory disease (PID) is a general term for infection of the female upper genital tract, including the uterus, Fallopian tubes, and ovaries. PID usually results from ascending infection from the vagina or the endocervix.
When infection spreads upwards from the cervix (entrance to the uterus), it causes one or more of the followings: 1- Endometritis: inflammation and infection of the endometrium. 2- Salpingitis: inflammation and infection of the fallopian tubes. 3- Oophoritis: inflammation and infection of the ovaries. 4- Salpingo-oophoritis. 5- Parametritis: inflammation and infection of the tissue around the uterus. 6- Tubo-ovarianabscess: a pocket of infected fluid in the ovary and fallopian tube. 7- Pelvicperitonitis: inflammation and infection of the peritoneum (lining of the inside of the abdomen). 8- Perihepatits.
Incidence: 1-2% of young sexually active women each year. The clinical symptoms usually begin with: 1- Acute phase, followed by either complete resolution or progress to 2- Chronic phase with further subacute or acute recurrences, or it may be 3- Clinically begins which is not recognized but damage has been done with subsequent infertility or ectopic pregnancy (silentPID).
Risk factors: PID most commonly develops in sexually active women. 1- Young age common in between 15-24 years of age. 2- Menstruation: intercourse during the period due to absence of cervical plug and vaginal acidity lowered by alkaline menstrual discharge. 3- During purperium: In adult women the genital tract defenses are weakest during and immediately after abortion and delivery because of raw placental site, breaks in the epithelial lining of the cervix and vagina, discharge of both liquor and lochia (both alkaline lead to decrease vaginal acidity), degenerated blood clots and fragments of decidua offer a nidus for infection and the patient s general resistance decrease by stress of pregnancy or by anemia and malnutrition.
4- Insertion of IUCD for the first three weeks after insertion. 5- Multiple partners. 6- Past history of STIs. 7- Termination of pregnancy. 8- HSG. 9- Smoking. 10- Vaginal douching and presence of foreign body. 11- Lack of contraceptive barrier. 12- Lower socio-economic group. 13- IVF and IUI and other surgical procedures. 14- Reinfection from untreated male partner (80%). 15- Genetic susceptibility to the disease.
Etiology PID is often polymicrobial, most often bacterial infection. Chlamydia and/or Gonorrhoea are the most common cause of PID. Other bacteria and viruses include Gardenerellavaginilis, Mycoplasmagenitalium, Mobiluncusspp. and other anaerobes, endogenousvaginalflora (anaerobicandaerobic), aerobicstreptococci, Mycobacteriumtuberculosis. Viruses such as H.simplex, echo, and coxackie viruses. May be due to fungal or parasitic infection. Mode of infection: Direct, lymphatic and haematogenous.
Acute PID Clinical features: PID may be symptomatic or asymptomatic. It ranges from subclinical endometritis to frank salpingitis, pyosalpinx, tubo-ovarian abscess, pelvic peritonitis and perihepatitis.
Suggestive symptoms of PID: 1- Lower abdominal pain - (usually bilateral), or pain around the pelvis. Perihepatitis causes right quadrant upper abdominal pain. 2- dyspareunia particularly of recent onset. 3- Abnormal vaginal bleeding intermenstrual and postcoital bleeding can occur secondary to associated cervicitis and endometritis. 4- Abnormal vaginal or cervical discharge as a result of associated cervicitis, endometritis or bacterial vaginosis. 5- Dysuria 6- Nausea and/or vomiting. 7- Pain in the rectum.
Physical signs: 1- Bilateral lower abdominal tenderness (sometimes radiating to the legs). 2- mucopurulant cervical discharge and cervicitis seen on speculum examination. 3- Cervical motion tenderness on bimanual vaginal examination. 4- adnexal tenderness on bimanual vaginal examination (with or without a palpable mass). 5- Fever> 38 C.
PID should be considered in a patient with the clinical signs and/or symptoms mentioned above or in an asymptomatic individuals.There are no single test for diagnosing PID. It is based on the symptoms, gynecological examination and investigations.
Investigations: 1- Pregnancy test ( -HCG) to exclude ectopic pregnancy as it may be confused with PID and early intrauterine pregnancy. 2- Endocervical swabs for chlamydia and gonorrhoea: a positive result supports the diagnosis of PID, but negative results do not exclude PID. 3- An elevated ESR and C-reactive protein (CRP) also support the diagnosis of PID, it is often normal in mild/moderate PID. 4- Elevated WBC count, may be normal in mild cases. 5- Screening for other STI especially those with positive results for gonorrhoea and chlamydia or patient at high risk for STI. The screen includes: Microscopy and/or culture for Trichomonasvaginalis. HIV antibody test. Syphillis serology. 6- Urinalysis and urine culture to exclude UTI.
Radiological investigations: 1- Transvaginal Ultrasound scanning: no definite feature for PID. It helps to exclude EP, ovarian cysts or appendicitis and can identify dilated fallopian tubes or tubal abscess. 2- Doppler: detect inflamed and dilated fallopian tubes and tubo-ovarian masses. 3- MRI and CT scanning: MRI can assist in making the diagnosis when there is difficulty. CT in acute PID may show obscuring of the pelvic planes, thickening of the uterosacral ligaments and accumulation of fluid in tubes and endometrial canal. In the upper abdomen it can provide evidence of perihepatitis
Surgical investigations: 1- Laparoscopy: may strongly support a diagnosis of PID but is an invasive procedure and the potential difficulty in identifying mild intra-tubal inflammation or endometritis, therefore it is not appropriate in routine clinical practice. It enables specimens to be taken from the fallopian tubes and the pouch of Douglas for bacterial culture, including gonorrhoea. Can provide information on the severity of the condition. Dilated hyperemic tubes with inflammatory, fibrinous exudates covering the tubes and the fundus of the uterus can be seen by laparoscopy.
15-30% of suspected cases may have no laparoscopic evidence of acute infection, despite organisms being identified from the fallopian tubes.When there is diagnostic doubt laparoscopy may, be useful to exclude alternative pathologies. 2- Endometrialbiopsy: There is insufficient evidence to support it as a routine diagnostic test at present.
Differential diagnosis 1- Ectopic pregnancy. 2- Acute appendicitis 3- Endometriosis. 4- Irritable bowel syndrome. 5- Complications of ovarian cyst. 6- Functional pain (pain of unknown physical origin). 7- UTI. 8- Inflammatory bowel disease
Management 1- Patients should be advised to avoid unprotected intercourse until they and their partners completed the treatment and follow-up. 2- Antibiotic therapy: Do not delay antibiotic treatment while waiting for the results of tests if PID is clinically suspected. Delayed treatment increases the risk of long-term complications.
3- General measures according to the severity of PID: - Rest is advised for those with severe disease. - If possibility of pregnancy, pregnancy test should be done to exclude ectopic pregnancy. - Restrict oral feeding - IV fluid to correct dehydration and acidosis. - Naso-gastric suction in the presence of distended abdomen or ileus. - Appropriate analgesia. - IV therapy is recommended for severe clinical disease.
Antibiotic treatment: Broad-spectrum antibiotic therapy is required to cover N. gonorrhoea, C. trachomatis, anaerobic infection and other possible pathogens. 1- In mildormoderatePID (in the absence of a tubo-ovarian abscess) there is no difference in outcome when women are treated as outpatients or admitted to the hospital provided there is no delay in treatment.
Outpatient antibiotic regimen: Oral ofloxacin 400 mg daily plus oral metronidazole 400 mg twice daily for 14 days. I.M ceftriaxone 250 mg single dose followed by oral doxycycline 100 mg twice daily plus metronidazole 400 mg twice daily for 14 days. Cefoxitin has a better evidence base for the treatment of PID than ceftriaxone if available. Alternative less strong treatment: IM ceftriaxone 250 mg immediately followed by azithromycin 1 g/week for 2 weeks.
Admission to hospital for parenteral therapy, observation, further investigations and/or possible surgical intervention should be considered in the following situations: >> Diagnostic uncertainty. >> Lack of response to oral therapy (3days). >> Inability to tolerate an oral therapy. >> Severe symptoms and signs (nausea, vomiting, fever > 39 C). >> Pregnancy (PID is rare in women with intrauterine pregnancy except in case of septic abortion) >> Presence of a tubo-ovarian abscess. >> Signs of pelvic peritonitis >> Inability to follow-up the patient.
Inpatient regimen Inpatient antibiotic treatment should be based on intravenous therapy which should be continued until 24 hours after clinical improvement and followed by oral therapy. Recommended regimens are: Ceftriaxone 2 g by IV infusion daily plus IV doxycycline 100 mg twice daily, followed by oral doxycycline 100 mg twice daily plus oral metronidazole 400 mg twice daily for a total of 14 days. IV clindamycin 900 mg three times daily plus IV gentamycin (2 mg/kg loading dose followed by 1.5 mg/kg three times daily or a single daily dose of 7 mg/kg) followed by either: Oral clindamycin 450 mg four times daily to complete 14 days.
OR -Oral doxycycline 100 mg twice daily plus oral metronidazole 400 mg twice daily to complete 14 days. - IV ofloxacin 400 mg twice daily plus metronidazole 500 mg three times daily for 14 days. -In inpatients the treatment response can be monitored by changes in CRP and WBC. -In severe cases and cases with failure of the initial treatment tubo-ovarianabscess should be excluded by vaginal U/S, CT or MRI. -All patients should be screened for STIs and HIV testing. -Oral metronidazole can be discontinued in those with mild to moderate PID if the patient is unable to tolerate it.
Surgical treatment Considered in severe cases or where there is clear evidence of a pelvic abscess not resolved by antibiotic therapy. Laparotomy/laparoscopy may help early resolution of the disease by division of adhesions and drainage of pelvic abscess. U/S-guidedaspiration of pelvic fluid collections is less invasive and may be equally effective. Depending on age and reproductive history, salpingo- oopherectomy done for extensive damage.
Follow-up 1- In the outpatient setting, review at 72hours is recommended, particularly for those with a moderate or severe clinical presentation. Failure to improve clinically suggests the need for further investigation, to exclude competing diagnoses, and may require admission for parenteral therapy and/or surgical intervention. 2- Further review 4-6weeks after therapy may be useful to ensure: - Adequate clinical response to treatment. - Compliance with oral antibiotics. - Screening and treatment of sexual contacts - Awareness of the significance of PID and its sequelae. - Repeat testing for chlamydia and gonorrhoea in those in whom persisting symptoms, compliance with antibiotics and/or tracing of sexual contacts indicate the possibility of persisting or recurrent infection.
Complications 1- Perihepatitis (Fitz-Hugh-Curtis syndrome). Occurs in up to 10-20% of women with PID. 2- Infertility: about one in 10 with a history of PID is infertile. The risk of infertility following PID is related to the number of episodes of PID and their severity. It doubles with each other episode. 3- Ectopic pregnancy: 1% if the woman had PID. 4- Chronic pelvic pain affects around 30%.
5- In pregnancy: PID is associated with an increase in preterm delivery, passing on the infection to the baby, and maternal and fetal morbidity. 6- Tubal occlusion, tubo-ovarian abscess (10%), and pelvic abscess. 7- Pelvic and generalized peritonitis. 8- Intestinal adhesions and obstruction. 9- Women with HIV may have more severe symptoms associated with PID. 10- In women with IUD in situ, consider removing it since this may be associated with better short term improvement in symptoms and signs. 11- Reiter s syndrome (reactive arthritis). 12- Recurrent PID.
Prevention 1- Use of barrier method, oral contraceptives, levonorgestrel-releasing intrauterine system (Merina). 2- Women at risk of STI such as chlamydia, set up a regular screening program if necessary. 3- If a woman have PID or STI advise her partner to be tested and, if necessary treated to prevent the spread of STI and recurrence of PID. 4- Avoid vaginal douching; douching upsets the delicate balance of bacteria in the vagina. 5- Proper hygiene habits. 6- Prophylactic antibiotics before instrumentation of the uterus.
Chronic pelvic inflammatory disease (PID) Chronic infection and inflammation of the internal genital organs is known as chronic PID. It is often started with acute or subacute infection (mostlyduetoSTI) with mild symptoms then it may produce chronic inflammation of the pelvic organs with scarring, adhesions, and tubal blockage. The damaged organs also become vulnerable to infection by other bacteria, so that chronic PID often involves multiple bacteria. Even with effective antibiotic treatment, long term resolution of chronic PID is difficult to achieve because the damaged tissues are easily re-infected. In some cases, the scarred tissue contains tiny collections of pus which are inaccessible to antibiotics and cause a recurrent exacerbation of disease.
Typically, chronic PID results in: The formation of adhesions frequently massive, between pelvic organs. This includes the uterus, fallopian tubes ovaries, bowel, bladder and pelvic side walls (frozen pelvis). The ovaries are frequently encased in scarring and tend to develop cysts. The tubes are typically blocked at their terminal end or in one or several points along its length (pyo-or hydrosalpinx) and tend to be enlarged with thick and inflamed walls.
Clinical features 1- Pelvic pain of variable pattern and severity (severe generalized or localized pain) which is crampy or constant, exacerbated by coitus and menstruation. 2- Deep seated dyspareunia. 3- Dysmenorhoea (congestive type). 4- Abdominal cramps and constipation due to bowel involvement in pelvic adhesions.
5- Rectal discomfort and backache. 6- Tendency for heavy periods or intermenstrual irregular bleeding. 7- There may be excessive cervical discharge (yellow). 8- Infertility only (is the role with chronic PID). 9- Intermittently, the chronic infection is complicated by acute episodes of disease characterized by fever and severe pain.
Examination: May reveal tenderness on one or both iliac fossa, with possible feeling of pelvic swelling on one or both sides. P/V: signs of chronic cervicitis, little enlargement of the uterus fixed in R/V. Tenderness on each side of pelvis with adnexal or pelvic mass.
Treatment 1- Conservative by antibiotic therapy, improvement of the general condition and analgesics if required. 2- Surgery: removal of the both ovaries and fallopian tubes with or without the uterus (hysterectomy) is indicated in: -Severe chronic pain or recurrent episodes of acute pain and fever. -Persistent symptoms such as dyspareunia and severe menorrhagia not responding to conservative therapy. -Persistence or gross enlargement of the pelvic masses despite conservative therapy. -In younger patients some healthy ovarian tissue can be preserved if present. -Surgery also indicated as differential diagnosis from other conditions.
Pelvic Tuberculosis (Tuberculous PID) -It is usually limited to patients from developing countries. It is now less common due to decline in pulmonary TB and early treatment of the disease. -It is almost always secondary to a focus elsewhere in the body. -It spread to the genital tract through blood stream usually from pulmonary lesion caused by the human type bacillus. Rarely the tube, ovaries and serousal layer of the uterus infected from T.B peritonitis or intestinal T.B caused by bovine or human type. -The primary infection ascends to the upper genital tract in 1-2% of cases. -Rarely genital TB can be sexually transmitted from a male with tuberculous epididymitis. -The fallopian tubes will be involved in 95-100% of cases, endometrium in 50-60%, ovaries in 20-30% and cervix, vagina and vulva in < 1%.
Signs & symptoms: 1- May be symptomless unless the patient complain from infertility in 45-55% of women, (due to either blockage of the fallopian tube or due to loss of tubal function even though the tubes are patent. 2- Menstrual disorders in 20% of cases especially excessive bleeding, secondary amenorrhoea, irregular cycle and post-menopausal bleeding. 3- Pain is uncommon unless secondary infection sets in. A secondary infection in tuberculoussalpingitis is characterized by all the symptoms of pyosalpinx (pain, nausea, vomiting and fever). 4- A tender, fixed mass is felt in the pelvis. 5- Blood stained vaginal discharge; post-coital bleeding, leucorrhoea, and painful ulcer are characteristic features of lower genital tract tuberculosis. 6- Poor general health in 25% of cases (weight loss, anorexia, night sweats and pyrexia).
Diagnosis: Confirmed by bacteriology. If infection in the F. tubes diagnosis by HSG or laparoscopy.
Treatment: 1- No need for hospitalization. Only those with fever and abdominal pain are admitted to the hospital in the initial stages of treatment. 2- The first line of treatment is with anti-tuberculardrugs. Isoniazid, rifampicin, pyrazinamide, ethambutol and/or streptomycin are the first line drugs given during the initial two-month phase of intensive drug therapy. 3- This is followed by a seven to ten months phase of drug therapy with isoniazid and rifampcin only. 4- Surgery is indicated if there is progression of disease, persistent pain and menorrhagia, persistent lesion, persistence of a large inflammatory mass (pyosalpinx and pyometra).
Prognosis: Nearly most early cases cured by chemotherapy. Fertility however, is resorted, in some cases, of those who conceive, 50% have tubal pregnancy, 20-30% abort. Only 2% of women with genital tuberculosis will have live birth.