Opioid Overdose and Prevention Methods
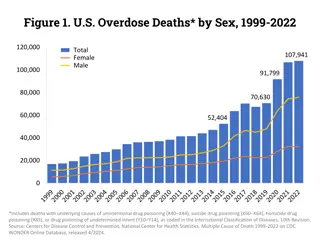
The World Health Organization defines opioid overdose as a condition that can lead to respiratory depression and death, often identified by pinpoint pupils, unconsciousness, and respiratory depression. The statistics show a concerning rise in opioid-related deaths, emphasizing the urgent need for prevention efforts. Various strategies such as education, monitoring programs, and law enforcement initiatives have been proposed to tackle the opioid crisis. Scientific reviews highlight the importance of provider education and overdose prevention programs.
Uploaded on Sep 15, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Part 3: Part 3: Prevention of Prevention of Opioid Overdose Opioid Overdose
Opioid Overdose Definition Opioid Overdose Definition - - World Health Organization World Health Organization Due to their effect on the part of the brain that regulates breathing, opioids in high doses can cause respiratory depression and death. An opioid overdose can be identified by a combination of three signs and symptoms referred to as the opioid overdose triad , which are: pinpoint pupils unconsciousness respiratory depression Combining opioids with alcohol and sedative medication increases the risk of respiratory depression and death, and combinations of opioids, alcohol, and sedatives are often present in fatal drug overdoses. SOURCE: https://www.who.int/substance_abuse/information-sheet/en/.
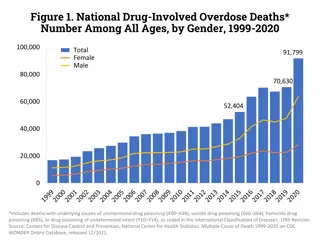
Drugs Involved in U.S. Overdose Deaths 1999 to 2017 Drug Overdose Deaths Drug Overdose Deaths Synthetic Opioids other than Methadone, 29,406 30,000 The most frequently mentioned drugs involved in these deaths: 25,000 Opioids: heroin, oxycodone, methadone, morphine, hydrocodone, and fentanyl 20,000 Heroin, 15,958 Natural and semi-synthetic opioids, 14,958 Cocaine, 14,556 15,000 Methamphetamine, 10,721 10,000 Benzodiazepines: alprazolam and diazepam 5,000 Stimulants: cocaine and methamphetamine Methadone, 3,295 0 2001 2009 2017 1999 2000 2002 2003 2004 2005 2006 2007 2008 2010 2011 2012 2013 2014 2015 2016 SOURCE: Hedegaard et al. (2018)
In 2016 1 in 65 deaths was opioid related. Among adults aged 25 to 34 years 1 in 5 deaths is opioid related. Among those aged 15 to 24 years, 12.4%of deaths were attributable to opioids. SOURCE: Gomes et al. (2018)
In 2017, 198 people died per day from drug overdoses- 10.2% increase from 2016 SOURCE: NCHS. (2018)
Review of Scientific Prevention Literature re: Opioid Crisis Review of Scientific Prevention Literature re: Opioid Crisis Prevention Education Provider Education Prescription Drug Monitoring Programs Law Enforcement Opioid Overdose Prevention Programs Review done by Dr. Wilson Compton and colleagues from NIDA SOURCE: Compton, Boyd, & Wargo. (2015)
10 Evidence-Based Strategies for Preventing Opioid Overdose - Naloxone Distribution -911 Good Samaritan Laws 911 Good Samaritan Laws SOURCE: https://www.cdc.gov/drugoverdose/pdf/pubs/2018-evidence-based-strategies.pdf.
WHO recommends that naloxone be made available to people likely to witness an opioid overdose, as well as training in the management of opioid overdose. Naloxone Naloxone Opiate antagonist Reverses or blocks the effects of other opioids Quickly restores normal respiration to a person whose breathing has slowed or stopped as a result of abusing heroin or prescription opioids Naloxone is short-acting Can be injected or inhaled through a nasal spray Auto-injectors approved in 2014 Least expensive method syringe and vial but that requires the most training SOURCE: DeSimone et al. (2018)
DOsupport the persons breathing by administering oxygen or performing rescue breathing. DOadminister naloxone. DOput the person in the recovery position on the side, if he or she is breathing independently. DOstay with the person and keep him/her warm. SOURCE: SAMHSA. (2018)
DON'Tslap or try to forcefully stimulate the person it will only cause further injury. If you are unable to wake the person by shouting, rubbing your knuckles on the sternum (center of the chest or rib cage), or light pinching, he or she may be unconscious. DON'Tput the person into a cold bath or shower. This increases the risk of falling, drowning or going into shock. DON'Tinject the person with any substance (salt water, milk, speed, heroin, etc.). The only safe and appropriate treatment is naloxone. DON'Ttry to make the person vomit drugs that he or she may have swallowed. Choking or inhaling vomit into the lungs can cause a fatal injury. SOURCE: SAMHSA. (2018)
Good Samaritan Laws Good Samaritan Laws As of July 15, 2017 All 50 states and DC passed legislation to improve laypersons access to naloxone 41 states and DC have passed legislation that provides some protection from arrest or prosecution for individuals who report an overdose SOURCE: The Network for Public Health Law. (2017)
Adoption of Naloxone Access and Overdose Adoption of Naloxone Access and Overdose Good Samaritan Laws Over Time Good Samaritan Laws Over Time SOURCE: The Network for Public Health Law. (2017)
Resources for Continued Learning Resources for Continued LearningOnline Naloxone Trainings https://www.getnaloxonenow.org/ http://getnaloxonenow.org>http://stopover dose.org/section/first-responders/ http://stopoverdose.org/section/first- responders/ http://prescribetoprevent.org/ https://store.samhsa.gov/system/files /information-for-prescribers.pdf https://store.samhsa.gov/system/files/ safety-advice-for-patients-family- members.pdf https://www.cdc.gov/drugoverdose/pdf/patient s/Preventing-an-Opioid-Overdose-Tip-Card-a.pdf