Mental Health Insights Among High-Income Countries Adults in 2016
Explore the prevalence of depression, anxiety, emotional distress, and socioeconomic needs among adults in high-income countries based on the 2016 Commonwealth Fund International Health Policy Survey. The data highlights the rates of mental health diagnoses, subjective experiences of emotional distress, socioeconomic challenges, and the hesitation towards seeking professional help for emotional distress.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
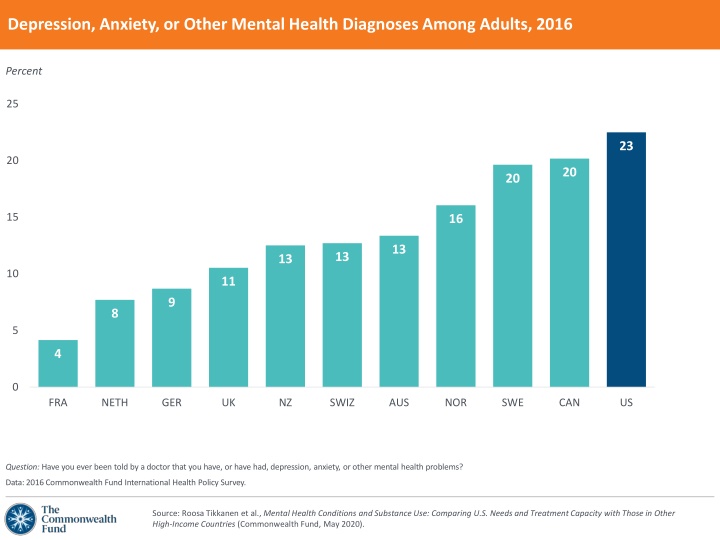
Depression, Anxiety, or Other Mental Health Diagnoses Among Adults, 2016 Percent 25 23 20 20 20 15 16 13 13 13 10 11 9 8 5 4 0 FRA NETH GER UK NZ SWIZ AUS NOR SWE CAN US Question: Have you ever been told by a doctor that you have, or have had, depression, anxiety, or other mental health problems? Data: 2016 Commonwealth Fund International Health Policy Survey. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Subjective Experience of Emotional Distress, 2016 Percent 50 40 30 27 26 24 20 21 21 20 20 19 17 10 12 7 0 GER FRA UK NETH NOR AUS SWIZ NZ SWE US CAN Question: In the past two years, have you experienced emotional distress, such as anxiety or great sadness, which you found difficult to cope with by yourself? Data: 2016 Commonwealth Fund International Health Policy Survey. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Socioeconomic Needs Among Adults Who Had and Had Not Experienced Emotional Distress, 2016 Percent who said always or usually * 50 Emotional distress No emotional distress 45 40 36 34 30 28 28 26 23 20 21 19 18 17 16 14 14 14 14 10 10 9 8 7 6 5 0 UK FRA GER NETH NOR SWE NZ SWIZ AUS CAN US Question:In the past 12 months, have you always or usually been worried or stressed about one or more of the following: having enough money to buy nutritious meals, crime or drugs in your neighborhood, and/or having enough money to pay your rent or mortgage? * Other response categories: sometimes, rarely, never. Data: 2016 Commonwealth Fund International Health Policy Survey. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Did Not Want to See a Professional for Emotional Distress, 2016 Percent who had experienced emotional distress 50 45 40 42 41 37 36 30 32 28 27 23 20 18 10 0 NOR US CAN FRA SWE NZ AUS UK SWIZ NETH Question: When you felt this way, were you able to get help from a professional when you needed it? Response: No, did not want to see a professional. Notes: Emotional distress refers to adults who report they have experienced anxiety or great sadness which they found difficult to cope with by themselves in the past two years. No data shown for GER because of small sample size (n<100). Data: 2016 Commonwealth Fund International Health Policy Survey. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Unable to Get or Afford Needed Mental Health Care, 2016 Percent who had experienced emotional distress 50 40 30 20 21 16 15 13 10 12 12 11 10 7 3 0 NETH NZ SWIZ CAN AUS UK SWE US NOR FRA Question: When you felt this way, were you able to get help from a professional when you needed it? Response: No, could not get help or could not afford to see a professional. Notes: Emotional distress refers to adults who report they have experienced anxiety or great sadness which they found difficult to cope with by themselves in the past two years. No data shown for GER because of small sample size (n<100). Data: 2016 Commonwealth Fund International Health Policy Survey. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Trends in Suicides, 19802016 Deaths per 100,000 (standardized rates) 2016 data: 30 US (13.9) FRA (13.1) 25 AUS (11.9) CAN (11.8) 20 NOR (11.6) NZ (11.5) 15 SWIZ (11.2) SWE (11.1) NETH (10.5) 10 GER (10.2) UK (7.3) 5 0 OECD average: 11.4 1980 1982 1984 1986 1988 1990 1992 1994 1996 1998 2000 2002 2004 2006 2008 2010 2012 2014 2016 Note: Rates reflect age- and sex-standardized rates for 2016 or latest available year (2015 for CAN, FRA; 2014 for NZ). Data: OECD Health Data 2019. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Deaths Related to Drug Use, 2016 Deaths per 1,000,000 (standardized rates) 12 10 10 9 8 8 6 4 OECD average: 3 4 3 3 3 3 3 2 2 1 0 NZ AUS NETH NOR SWE UK FRA CAN SWIZ US GER Notes: Reflects deaths from psychoactive substance use, including from opioids, cannabis, sedatives, hypnotics, anxiolytics, cocaine, other stimulants, hallucinogens, nicotine, inhalants, and other psychoactive substances, but excluding alcohol. Rates reflect age- and sex-standardized rates for 2016 or latest available year (2015 for CAN, FRA; 2014 for NZ). Data: OECD Health Data 2019. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Mental Health Workforce Supply, 2017 Number of professionals working in the mental health sector, per 100,000 population 300 Psychiatrists 277 Nurses 15 250 Psychologists 221 69 Social workers 207 200 14 44 168 49 144 21 150 91 122 21 93 104 105 100 11 98 48 4 29 71 63 30 145 123 21 13 103 50 84 75 74 60 51 50 49 0 CAN SWIZ AUS FRA NETH NOR US NZ SWE GER Notes: Data for 2017 or latest available year (2016 for NZ, NOR, SWE, US; 2015 for AUS, GER, NETH, SWIZ). No data available for UK. Because of rounding, the total number of professionals may not equal the sum of the four subcategories of workers. Data: World Health Organization Global Health Observatory data repository. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Primary Care Practices with Psychologists or Mental Health Providers on Team, 2019 Percent 100 94 93 80 60 56 40 41 33 33 31 31 20 14 13 5 0 NETH SWE AUS CAN NZ US FRA UK NOR SWIZ GER Note: Data reflect the share of primary care physicians who indicated that a psychologist or mental health provider work on their team to provide patient care. Data: 2019 Commonwealth Fund International Health Policy Survey of Primary Care Physicians. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).
Primary Care Practice Preparedness to Manage Patients with Mental Illnesses or Substance Use Related Issues, 2019 Percent who said they were well prepared * 100 Mental illnesses Substance use related issues 80 84 74 73 66 66 60 63 61 57 56 44 46 40 30 27 24 23 31 21 20 20 18 20 13 13 0 NETH AUS NOR NZ GER SWIZ CAN SWE UK US FRA Note: Reflects primary care physicians who reported that their practices are well prepared, with respect to having sufficient skills and experience, to manage care for patients with mental illnesses (e.g., anxiety, mild or moderate depression) or substance use related issues (e.g., drug, opioid, alcohol use). * Other response categories: somewhat prepared, not prepared. Data exclude those who said do not see these patients (0 2% for mental illness; <1% 10% for substance use related issues). Data: 2019 Commonwealth Fund International Health Policy Survey of Primary Care Physicians. Source: Roosa Tikkanen et al., Mental Health Conditions and Substance Use: Comparing U.S. Needs and Treatment Capacity with Those in Other High-Income Countries (Commonwealth Fund, May 2020).