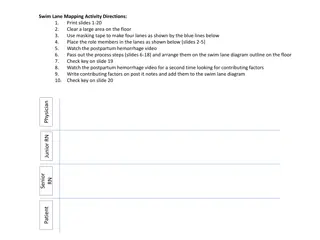
Management of Postpartum Patient with Persistent Tachycardia and Dizziness
A 33-year-old African American female at 39 weeks of gestation, G4P3, with possible ITP and anemia, was admitted for induction. Following delivery, her vital signs and labs were stable initially, but she developed persistent tachycardia and mild dizziness postpartum. After transfusion and monitoring, her symptoms persisted, leading to further evaluation and monitoring before eventual discharge.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Case Presentation Dr. Berry Campbell Project ECHO SC Pregnancy Wellness Wednesday, July 21, 2021
33 yo AA female at 39 weeks G4P3 Admitted for induction BMI 26 Hx possible ITP, never treated (followed by heme-onc) No prior surgeries
OB Hx: SVD term x 3, largest 8#4; smallest 6#. Hx pp hemorrhage 3rddelivery EFW 7#6 No prior surgeries Anemia Hb 7.9 pre-delivery
Admission vitals BP 110/60, P 110, normal resp rate Labs: Hb 7.9; plt 166K; WBC 8K T&C 2 units FHT reactive, spontaneous ctx every 5-8 minutes
Labor unremarkable 7#12 apgars 8/9 EBL 400ml Vitals: pulse 122 after delivery; BP 100/60, O2 sats 99% No symptoms Management?
Transfused 2 uPRBC, CBC ordered following morning Pp #1 P124; BP 100/58; O2 sats 99%; afebrile No complaints Labs: Hb 9.9, WBC 5K; plt 145K PxEx: FF and nontender; lochia normal
PP #2no complaints PxEx unchanged Ready for discharge Called to see her for pulse persistently >125, BP 95-110/50-60, afebrile. C/O mild dizziness when up PLAN?
Labs ordered: CBC Orthostatics ordered: normal Hb 10.2, plt 135K, WBC 4.5K PxEx no change, O2 sats normal, afeb Plan?
Decided to observe another day PP #3 alert, no c/o except fast heart rate Labs: Hb 11.2, plt 122K, WBC 3.6K Afeb, pulse 132, RR <20, O2 sats 98%; good UOP Exam abd nontender, fundus firm, no edema Pt insists on discharge Plan?
Asked hematology to see her (9am) Reassured Decided to watch and repeat labs later, discharge if remained normal. OB assessed twice through the morning (10 & 1130am), no changes Later decided to give abs empirically (rocephin), ordered 3pm Went to draw labs at 5pm, patient confused Thoughts?
Called OB to assess (5pm) and was in a delivery. Rapid called by nursing 15 minutes later (5:15pm)
ER physician ran code, intubated Labs: WBC 2K, Hb 12, plt 92K, Cr 2.6, AST 120 Abs and pressors given Unsuccessful resuscitation Maternal death 1 hour after intubation Diagnosis: Septic shock
Thoughts? Lactate > 4 during code Cultures-group A sepsis (puerperal sepsis)
Sepsis Life-threatening organ dysfunction caused by dysregulated host response to infection
Sepsis Emphasis MUST BE ON organ dysfunction, NOT signs of infection
Septic Shock Subset of sepsis where underlying circulation and cellular/metabolic abnormalities are profound enough to substantially increase mortality Sepsis with persistent hypotension requiring vasopressors to maintain MAP>65 + lactate > 2mmol/L
Management Cultures Serum lactate Antibiotics within 1 hour of suspicion Fluids (carefully 1-2 L) Vasopressors
Group A strep sepsis Child-bed fever Puerperal sepsis Pre-antibiotic era, common cause of death Not as common today BUT presentation is erratic and confuses Rec: empiric abs can save lives in situations that are unclear Full lab panels INCLUDING lactate
Tachycardia and leukocytosis common in pregnancy and postpartum under-action by OB team