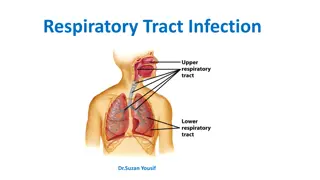
Lower Respiratory Tract Infections
Lower respiratory tract infections can vary from bronchitis to pneumonia, with severe cases leading to life-threatening airway obstruction. Learn about the classification, differential diagnosis, and management of these infections.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
LOWER RESPIRATORY TRACT INFECTIONS Tomasz Brzeski
Classification of respiratory infections Upper respiratory tract infection Laryngeal/tracheal infection Bronchitis/Bronchiolitis Pneumonia
Classification of respiratory infections Upper respiratory tract infection Laryngeal/tracheal infection Bronchitis/Bronchiolitis Pneumonia.
Laryngeal/tracheal infections The mucosal inflammation and swelling produced by laryngeal and tracheal infections can rapidly cause lifethreatening obstruction of the airway in young children.
Differential diagnosis of acute upper airways obstruction Viral laryngotracheobronchitis also known as croup - the most frequent cause Epiglottitis Bacterial tracheitis Inhalation of smoke and hot air in fires Trauma to the throat Retropharyngeal abscess Laryngeal foreign body Allergic laryngeal angioedema Infectious mononucleosis causing severe lymph node swelling Measles Diphtheria
Acute upper airways obstruction - SYMPTOMS Stridor - heard predominantly on inspiration Hoarseness due to inflammation of the vocal cords A barking cough A variable degree of dyspnoea
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT Fast medical history Physical examination Pulse oximetry Oxygen Adrenaline in oxygen nebulization Budezonide in nebulization Intravenous line Intravenous steroids if necessary
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT FAST MEDICAL HISTORY onset of illness, preceding coryza, cough, fever, able to drink, vaccination, allergies FAST MEDICAL EXAMINATION general apperance, breath and heart rate, chest retraction (none, only on crying, at rest), stridor (none, only on crying, at rest), central cyanosis, drowsiness, deterioration, drooling saliva,pulse oximetry Do not examine pharynx by spatula if you think about the epiglottis risk of total obstruction of upper airways.
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT IN SEVERE UPPER AIRWAYS OBSTRUCTION MEDICAL HISTORY AND MEDICAL EXAMINATION SHOULD TAKE LESS THAN 1 MINUTE IN THE SAME TIME OTHER STAFF OF EMERGENCY DEPARTMENT (NURSE, PARAMEDIC) PREPARE ADRENALINE IN OXYGEN NEBULIZATION.
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT DRUGS: 1 ) Adrenaline in nebulization: < 1 year - 1 mg > 1 year - 2 mg 2) Budesonide in nebulization: < 1 year - 1 mg > 1 year - 2 mg 3) Hydrocortison i.v.: 8-10 mg/kg/dose
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT What do you think? When is the right moment to place an intravenous line?
Acute upper airways obstruction What should a doctor do in EMERGENCY DEPRATMENT When you do not see a child (e.g. telephone consultation in emergency depratment/night ambulatory) and medical history suggest that the severe upper airway obstruction is a reason of the problem (parents usually do not have any medication or nebulizator) the best advice: PROVIDE A CHILD COLD AIR IMMEDIATELY GO TO THE HOSPITAL\ CALL 112
Croup (laryngotracheobronchitis) Viral croup accounts for over 95% of laryngotracheal infections Parainfluenza viruses are the commonest cause, rarely human metapneumovirus, RSV and influenza, but they can produce a similar symptoms Croup occurs from 6 months to 6 years of age but the peak incidence is in the second year of life It is commonest in the autumn The typical features are a barking cough, harsh stridor and hoarseness, usually preceded by coryza The symptoms often start, and are worse, at night
Epiglottitis Epiglottitis is a lifethreatening emergency due to the high risk of respiratory obstruction It is caused by H. influenzae type b In many countries (included Poland :)), the introduction of Hib vaccination in infancy has led to a >99% reduction in the incidence of epiglottitis and other invasive H. influenzae type b infections There is intense swelling of the epiglottis and surrounding tissues associated with septicaemia Epiglottitis is most common in children aged 1 6 years but affects all age groups It is important to distinguish clinically between epiglottitis and croup, as they require quite different treatment.
Over days Severe, barking YES Unwell <38,5 Harsh Hoarse Croup Epiglottitis Over hours NO Absent, silent NO YES Toxic >38,5 Soft Muffled Onset Preceding coryza Cough Able to drink Drooling saliva Apperance Fever Stridor Voice YES NO
Classification of respiratory infections Upper respiratory tract infection Laryngeal/tracheal infection Bronchitis/Bronchiolitis Pneumonia
BRONCHIOLITIS -ETIOLOGY Bronchiolitis is a disease of small bronchioles with increased mucus production and occasional bronchospasm, sometimes leading to airway obstruction. It is most commonly caused by a viral lower respiratory tract infection.
BRONCHIOLITIS -ETIOLOGY Bronchiolitis is most commonly seen in infants and young children, with most severe cases occurring among infants. Bronchiolitis is potentially life-threatening. Respiratory syncytial virus (RSV) is a primary cause of bronchiolitis Viral bronchiolitis is extremely contagious and is spread by contact with infected respiratory secretions.
BRONCHIOLITIS - EPIDEMIOLOGY Bronchiolitis is a leading cause of hospitalization of infants. Bronchiolitis occurs almost exclusively during the first 2 years of life, with a peak age at 2 to 6 months. In the United States, annual peaks are usually in the late winter months from December through March
BRONCHIOLITIS - SYMPTOMS Bronchiolitis caused by RSV has an incubation period of 4 to 6 days. Bronchiolitis classically presents as a progressive respiratory illness similar to the common cold in its early phase with cough and rhinorrhea. It progresses over 3 to 7 days to noisy, raspy breathing and audible wheezing. There is usually a low-grade fever accompanied by irritability, which may reflect the increased work of breathing. In contrast to the classic progression of disease, young infants infected with RSV may not have a prodrome and may have apnea as the first sign of infection.
BRONCHILITIS - LABORATORY AND IMAGING Routine laboratory tests are not required to confirm the diagnosis Pulse oximetry is adequate for monitoring oxygen saturation Chest radiographs frequently show signs of lung hyperinflation,including increased lung lucency and flattened or depressed diaphragms
BRONCHOLITIS - PROGNOSIS Most hospitalized children show marked improvement in 2 to 5 days with supportive treatment alone There is a 1% to 2% mortality rate
BRONCHOLITIS - PREVENTION Monthly injections of palivizumab, an RSV-specific monoclonal antibody, initiated just before the onset of the RSV season confers some protection from severe RSV disease. Palivizumab is indicated for some infants under 2 years old with chronic lung disease, very low birth weight, and those with hemodynamically significant cyanotic and acyanotic congenital heart disease. Immunization with influenza vaccine is recommended for all children older than 6 months and may prevent influenza-associated disease.
Whooping cough = pertussis Classic pertussis (whooping cough) is caused by Bordatella pertussis, a gram-negative pleomorphic bacillus. Bordatella pertussis infects only humans and is transmitted person to person by coughing. The incubation period is 7 to 10 days. Patients are most contagious during the first 2 weeks of cough.
Whooping cough Classic pertussis is seen in children between 1 and 10 years old. The progression of the disease is divided into catarrhal, paroxysmal, and convalescent stages.
Whooping cough - SYMPTOMS The catarrhal stage is marked by nonspecific signs (increased nasal secretions and low-grade fever) lasting 1 to 2 weeks. The paroxysmal stage is the most distinctive stage of pertussis and lasts 2 to 4 weeks. Coughing occurs in paroxysms during expiration, causing young children to lose their breath. The forceful inhalation against a narrowed glottis that follows this paroxysm of cough produces the characteristic whoop. Posttussive emesis is common. The convalescent stage is marked by gradual resolution of symptoms over 1 to 2 weeks. Coughing becomes less severe, and the paroxysms and whoops slowly disappear.
Whooping cough - SYMPTOMS Although the disease typically lasts 6 to 8 weeks, residual cough may persist for months, especially with physical stress or respiratory irritants. Infants may not display the classic findings, and the first sign in the neonate may be apnea. Young infants are unlikely to have the classic whoop, more likely to have central nervous system damage as a result of hypoxia, and more likely to have secondary bacterial pneumonia.
Whooping cough LABORATORY TESTS LEUKOCYTOSIS increased white blood cell count from 20,000 cells/mm3 to more than 50,000 cells/mm3 with LYMPHOCYTOSIS
Whooping cough TREATMENT MACROLIDE ANTIBIOTICS !!! Clarithromycin Azithromycin Erythromycin
Whooping cough PREVENTION VACCINATION !!! Do you know how look like the vacination program against whooping cough in Poland?
Classification of respiratory infections Upper respiratory tract infection Laryngeal/tracheal infection Bronchitis/Bronchiolitis Pneumonia
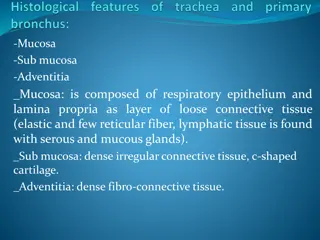
PNEUMONIA - DEFINITON Pneumonia is an infection of the lower respiratory tract that involves the airways and parenchyma with consolidation of the alveolar spaces. The term lower respiratory tract infection is often used to encompass bronchitis, bronchiolitis, pneumonia, or any combination of these three.
PNEUMONIA - DEFINITON Lobar pneumonia describes pneumonia localized to one or more lobes of the lung. Atypical pneumonia describes patterns typically more diffuse or interstitial than lobar pneumonia. Bronchopneumonia refers to inflammation of the lung that is centered in the bronchioles and leads to the production of a mucopurulent exudate that obstructs some of these small airways and causes patchy consolidation of the adjacent lobules. Interstitial pneumonitis refers to inflammation of the interstitium, which is composed of the walls of the alveoli, the alveolar sacs and ducts, and the bronchioles. Interstitial pneumonitis is characteristic of acute viral infections but also may be a chronic inflammatory or fibrosing process.
PNEUMONIA - DEFINITON Community-acquired pneumonia (CAP) is acquired in the community, outside of health care facilities. Compared with hospital-acquired pneumonia, it is less likely to involve multidrug-resistant bacteria. Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48 72 hours after being admitted. It is usually caused by a bacterial infection, rather than a virus.
Pneumonia - PATHOGENS 1-21 day of life Bacteria: Streptococcus group B (Streptococcus agalactiae), Enterobacteriaceae, Listeria monocytogenes Viruses: CMV, rubella, HSV, enteroviruses 22 day of life- 3 months Bacteria: Streptococcus pneumoniae, Chlamydia trachomatis, Bordaetella pertussis, Staphylococus aureus, Ureaplasma urealyticum Viruses: RSV, hMPV, influenza, parainfluenza, adenoviruses 4 months-4 years Viruses: RSV, hMPV, adenoviruses, influenza, parainfluenza, rhinoviruses Bacteria:Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Chlamydophila pneumoniae > 5 years Bacteria: Streptococcus pneumoniae, Mycoplasma pneumoniae, Chlamydophila pneumoniae Viruses: influenza, adenoviruses, parainfluenza, RSV, rhinoviruses
ATYPICAL PNEUMONIA What bacteria are responisble for atypical pneumonia? Mycoplasma pneumoniae Chlamydophila pneumoniae Chlamydia trachomatis Ureaplasma urealyticum Legionella pneumophila
PNEUMONIA - SYMPTOMS Fever Dyspnea Tachypnoe Cough Chest pain Abdominal pain Child with atypical pneumonia often has no fever, more often has got wheezing.
PNEUMONIA - DIAGNOSIS Medical history (oneset of illness, fever, cough, difficulty in breathing, chest or abdominal pain) Physical examination (the best clinical sign of pneumonia in children is increased respiratory rate - pneumonia can sometimes be missed if the respiratory rate is not measured in a febrile child, nasal flaring,chest retraction, endinspiratory respiratory coarse crackles over the affected area or decreased breath sounds and bronchial breathing over the affected area, oxygen saturation may be decreased Laboratory test (increased inflamatory indicators, acidemia) Chest X-ray (may confirm the diagnosis, but with the exception of a classic lobar pneumonia characteristic of Streptococcus pneumoniae, a chest Xray cannot be differental tool between bacterial and viral pneumonia.
When admission to a hospital is necessary? Age < 6 month Hipoxemia (oxygen saturation <92%) Tachypnoe Severe general condition Respiratory or cardiovascular failure Neurological symptoms (e.g. convulsions, disturbances of consciousness) Chronic illness (diabetes melitus, neoplasm, immunological disorders, kidney or liver disorders) Granulocytopenia Large changes in chest x ray Complications of pneumonia (parapneumonic effusion or an empyema, abscessus of the lung) Social reasons
PNEUMONIA - TREATMENT Antibiotic therapy Symptomatic therapy Hydratation oral/i.v. Salbutamol in pMDI/nebulization Ipratropium bromide in nebulization Steroids i.v./pMDI/nebulization Mucolitics Antypyretic drugs
Pneumonia Antibiotic therapy 1-21 day of life Ampicilin with aminoglycoside antibiotic or 3rd generation cephalosporin 22 day of life- 3 months Amoxicillin or Cefuroxime or Amoxicillin with Clavulanate Atypical ethiology: Macrolide antibiotic 4 months-4 years Good general condtition without antibiotic If antibiotic is necessery - first line therapy: Amoxicillin Atypical ethiology: Macrolide antibiotic > 5 years Amoxicillin or Macrolide antibiotic Severe symptoms/hospitalization B-lactam antibiotic + Macrolide
PNEUMONIA- COMPLICATIONS Bacterial pneumonias frequently cause inflammatory fluid to collect in the adjacent pleural space, causing a parapneumonic effusion or, if grossly purulent, an empyema. Small effusions may not require any special therapy. Large effusions may restrict breathing and require drainage. Scarring of the airways and lung tissue may leave dilated bronchi, resulting in bronchiectasis and increased risk for recurrent infection. Pneumonia that causes necrosis of lung tissue may evolve into a lung abscess. Lung abscess is an uncommon problem in children.
PNEUMONIA- PROGNOSIS Most children recover from pneumonia rapidly and completely, although radiographic abnormalities may take 4 to 8 weeks to return to normal. In some cases, the possibility of underlying disease must be investigated further, such as with tuberculin skin test, sweat chloride determination for cystic fibrosis, serum immunoglobulin and IgG subclass determinations, bronchoscopy to identify anatomic abnormalities or foreign body, and barium swallow for gastroesophageal reflux. Severe adenovirus pneumonia may result in bronchiolitis obliterans, a subacute inflammatory process in which the small airways are replaced by scar tissue, resulting in a reduction in lung volume and lung compliance.
Pneumonia - PREVENTION FOR EVERYBODY: VACCINATION !!! THINKING IN HIGH RISK PATIENTS: Palivizumab FOR HOSPITAL STAFF: Hand washing before and after contact with patient Gloves for invasive procedure Good microbiology policy and procedure