Irritable bowel syndrome(IBS)
Irritable Bowel Syndrome (IBS) is a common gastrointestinal condition characterized by recurrent abdominal pain, abnormal defecation, and changes in stool frequency and form. It can significantly impact a person's quality of life. This condition can be differentiated from other GI syndromes by assessing symptoms, using Rome criteria, and considering the absence of alarm symptoms. Diagnosis often involves a combination of medical history, physical examination, and possibly additional tests. Treatment options may include dietary modifications, medication, and behavioral therapies, depending on the individual's symptoms and needs.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Objectives: At the end of this lecture, the student must be able to : Know what is IBS ? What is Rome criteria ? How can differentiate IBS from other GI syndromes ? How can approach to a patient suspected to have IBS ?
30 year old female patient with history of depression presented with 6 months history of recurrent abdominal pain , pain relief on defecation associated with change in form and stool frequency , no nocturnal symptoms, no wt. Loss , the examination is non remarkable What is the most cause of her current complain ? A. COELIAC DISEASE B. IRRITABLE BOWEL SYNDROME C. ULCERATIVE COLITIS D. CROHN DISEASE E. CHRONIC PANCREATITIS
55 year old male patient presented with six months history of nonspecific abdominal pain that relief with defecation associated with altered bowel habit between hard and loss stool during that period, there is no bleeding per rectum , no fever, no weight loss, the patient undergo investigation that reveal the following: Hb%=9.9g/dl ESR=60 WBC=7000 Platelets=250000/ml TSH =1.9Mmol/L (N=0.5-5Mmol/L) What is the best next step? A. Initiate treatment with antispasmodic drugs B. Initiate treatment with tricyclic antidepressant C. Send the patient for lower endoscopy D. Initiate dietary modification E. refer for cognitive behavioral therapy
A 30 year old woman has a diagnosis of diarrhoea-predominant IBS. Her symptoms are negatively impacting her ability to work in the local supermarket and she is avoiding social functions for fear of unpredictable onset of symptoms. She has tried a variety of dietary manipulations including a wheat-exclusion diet, a dairy-free diet and avoidance of caffeinated drinks, with no improvement of her symptoms. What is the next most appropriate treatment to consider? A. 5-HT4 agonist, prucalopride B. Nocturnal small-dose diazepam C. Peppermint capsule D. Probiotics E. Referral to dietician for consideration of a low-FODMAP (fermentable oligo-, di- and monosaccharides, and polyols) diet
Regarding irritable bowel syndrome, all of the following support the diagnosis of IBS except? A. Absent of weight loss B. Abdominal pain relief by defecation C. Change in stool form D. High erythrocytes sedimentation rate (ESR) E. change in frequency of stool
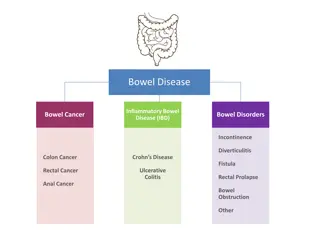
INTRODUCTION INTRODUCTION characterised by recurrent abdominal pain in association with abnormal defecation in the absence of a structural abnormality of the gut. About 10 15% of the population are affected at some time but only 10% of these consult their doctors because of symptoms. the most common cause of gastrointestinal referral and accounts for frequent absenteeism from work and impaired quality of life. Young women are affected 2 3 times more often than men. Coexisting conditions, such as non-ulcer dyspepsia, chronic fatigue syndrome, dysmenorrhoea and fibromyalgia, are common. sometimes associated with a history of physical or sexual abuse
Pathophysiology Pathophysiology Incompletely understood Different factors play a role in the pathophysiology : 1. Behavioural and psychosocial factors: Acute psychological stress and overt psychiatric disease are known to alter visceral perception and gastrointestinal motility. About 50% of patients referred to hospital have a psychiatric illness, such as anxiety, depression, somatisation and neurosis. Panic attacks are also common. Increased prevalence of abnormal illness behaviour, with frequent consultations for minor symptoms and reduced coping ability
2.Physiological factors: IBS may be a serotoninergic (5-HT) disorder, as evidenced by relatively excessive release of 5-HT in diarrhoea-predominant IBS (D-IBS) and relative defciency with constipation- predominant IBS (C-IBS). 5-HT3 receptor antagonists are effective in D-IBS, while 5-HT4 agonists improve bowel function in C-IBS. IBS may represent a state of low-grade gut inflammation or immune activation, not detectable by tests, with raised numbers of mucosal mast cells that sensitise enteric neurons by releasing histamine and tryptase. Immune activation may be associated with altered CNS processing of visceral pain signals. This is more common in women and in D-IBS, and may be triggered by a prior episode of gastroenteritis with Salmonella or Campylobacter species.
3. Luminal factors 3. Luminal factors Both quantitative and qualitative alterations in intestinal bacterial microbiota (gut dysbiosis )have been reported, this is supported by the development of symptoms in patients with SIBO and the response to nonabsorpable antibiotic( Refaximin). Dietary factors are also important. Some patients have chemical food intolerances (not allergy) to poorly absorbed, short-chain carbohydrates (lactose, fructose and sorbitol, among others), collectively known as FODMAPs (fermentable oligo-, di- and monosaccharides, and polyols. Non-coeliac gluten sensitivity (negative coeliac serology and normal duodenal biopsies) seems to be present in some IBS patients. intolerant of chemicals such as salicylates or benzoates, found in certain foods.
Clinical features Clinical features The cardinal feature of IBS is the recurrent abdominal discomfort, that is : Colicky or cramping in nature. Felt in the lower abdomen. Relieved by defecation. Abdominal bloating worsens throughout the day; the cause is unknown but it is not due to excessive intestinal gas. Altered bowel habits : Mostly have alternate between episodes of diarrhoea and constipation(mixed type). Some have diarrhea predominant Some have constipation predominant
Constipation predominant type IBS: Tend to pass infrequent pellety stools in association with abdominal pain or proctalgia Diarrhea predominant IBS: frequent defecation but produce low-volume stools Absent to rarely occurrence of nocturnal symptoms Passage of mucus is common but rectal bleeding does not occur In IBS : NO Wt. loss NO Nocturnal symptoms NO Rectal bleeding No fever constitutionally well patient Physical examination is generally unremarkable, with the exception of variable tenderness to palpation
Diagnostic criteria for IBS Rome III criteria for diagnosis of irritable bowel syndrome: Recurrent abdominal pain or discomfort on at least 3 days per month in the last 3 months, associated with two or more of the following: Improvement with defecation Onset associated with a change in frequency of stool Onset associated with a change in form (appearance) of stool . Supporting diagnostic features for IBS: Presence of symptoms for more than 6 months Frequent consultations for non-gastrointestinal problems Previous medically unexplained symptoms Worsening of symptoms by stress.
Alarm features for IBS Age > 50 years; male gender Weight loss Nocturnal symptoms Family history of colon cancer Anaemia Rectal bleeding
Investigations: The diagnosis of IBS is clinical and can be make with confident by the application of the Rome criteria combined with the absent of alarm of symptoms. Investigations need to be done in atypical presentations in order to exclude other gastrointestinal diseases, like CBC with ESR, CRP, Stool for calprotectin with or without sigmoidoscopy , all of these investigations are normal in IBS. Colonoscopy should be undertaken in older patients (over 40 years of age) to exclude colorectal cancer. Diarrhoea-predominant patients justify investigations to exclude coeliac disease microscopic colitis lactose intolerance bile acid diarrhoea thyrotoxicosis and, in developing countries, parasitic infection
RISK FACTORS for IBS RISK FACTORS for IBS The best-accepted risk factor for IBS is bacterial gastroenteritis. The risk of postinfection IBS has been reported to be increased with depression, adverse life events and hypochondriasis, female gender, younger age, and prolonged duration of diarrhea following the initial attack. Bacterial virulence factors also may be important, but IBS also can follow non-bacterial enteritis, including viral gastroenteritis, and infection with Trichinella, or Giardia. Other risk factors for IBS include: an affluent childhood environment, premenopausal and postmenopausal estrogen use, recent antibiotic use, food intolerance extraintestinal somatic symptoms, and poor quality of life (QOL). IBS runs in families, and low birth weight is also a risk factor for IBS, even after controlling for genetic influences.
Management The most important steps are to make a positive diagnosis and reassure the patient. A cycle of anxiety leading to colonic symptoms,which further heighten anxiety, can be broken by explaining that symptoms are not due to a serious underlying disease but instead are the result of behavioural, psychosocial, physiological and luminal factors. Dietary management: Eat regularly and avoid missing meals Take time to eat Ensure adequate hydration and avoid carbonated and caffeinated drinks Reduce alcohol intake Reduce intake of resistant starch and insoluble fiber Avoid foods with artificial sweeteners Consider a wheat-free diet Consider a lactose exclusion diet Consider a diet low in FODMAPs Probiotics, in capsule form, can be effective if taken for several months
Patients with intractable symptoms sometimes benefit from several months of therapy with a tricyclic antidepressant, such as amitriptyline or imipramine (10 25 mg orally at night). Side-effects include dry mouth and drowsiness but these are usually mild and the drug is generally well tolerated. It may act by reducing visceral sensation and by altering gastrointestinal motility. Anxiety and affective disorders may also require specific treatment. The 5-HT4 agonist prucalopride, the guanylate cyclase-C receptor agonist linaclotide, and chloride channel activators, such as lubiprostone, can be effective in constipation predominant IBS. Trials of anti-inflammatory agents, such as ketotifen or mesalazine, and the antibiotic rifaximin may be considered
Psychological interventions, such as cognitive behavioural therapy, relaxation and gut-directed hypnotherapy, should be reserved for the most difficult cases. A range of complementary and alternative therapies exist; most lack a good evidence base but are popular and help some patients . Most patients have a relapsing and remitting course. Exacerbations often follow stressful life events, occupational dissatisfaction and difficulties with interpersonal relationships.