Improving Hospital Journey for People with Disabilities
This content delves into the challenges faced by individuals with disabilities during hospital stays, emphasizing the importance of communication, rights, and the impact of personal attitudes. It highlights the rights outlined in Article 25 of the United Nations Convention, the NSW Disability Inclusion Act 2014, and the NSW Health Disability Inclusion Action Plan. People with intellectual disabilities are particularly vulnerable to adverse outcomes in healthcare settings. The aim is to enhance the hospital experience for individuals with disabilities by promoting positive attitudes, creating accessible environments, and providing equitable support services.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Admission2Discharge Together Improving the hospital journey for people with Disability
Aim Improve the hospital journey for people with disability
Learning Outcomes Challenges that a person with disability may experience in hospital Rights of people with disability Importance of communication How personal perceptions, values and attitudes impact on the care and support provided to a person during their hospitalisation Purpose of TOP 5 and the Admission2Discharge Together (A2D) Folder.
Article 25 of the United Nations Convention The rights of Persons with Disability Persons with disabilities have a right to the enjoyment of the highest attainable standard of health without discrimination on the basis of disability.
NSW Disability Inclusion Act 2014 Acknowledges that people with disability have the same human rights as other members of the community. Enables people with a disability to exercise choice and control in the pursuit of their goals and the planning and delivery of their supports and services. Provide safeguards in relation to the delivery of supports and services for people with disability. Supports the purposes and principles of the United Nations Convention on the Rights of Persons with Disability.
NSW Health Disability Inclusion Action Plan Four Focus Areas 1. Promoting positive attitudes and behaviours 2. Creating liveable environments 3. Providing equitable systems and processes 4. Supporting access to meaningful employment opportunities
People with intellectual disability Experience high rates of adverse outcomes during hospital stays Experience poorer health outcomes overall Have more difficulty in obtaining the necessary health services in comparison with other populations Khran & Drum 2007 Experience significant medical and mental problems Conditions often unrecognised, misdiagnosed and poorly managed AIHW 2008;Lennox & Kerr
Ombudsman NSW Report of Reviewable Deaths in 2014,2015,2016 and 2017 Deaths of people with disability in residential care (2018) 2014-17, the deaths of 494 people with disability in care were reviewed. 64% of deaths were sudden and unexpected On average people were 55 years old when they died, 25 years younger than the general population
Leading causes of death Nervous system disease (16.1%) mainly epilepsy and cerebral palsy Respiratory diseases (15.5%) mainly pneumonia and aspiration pneumonia Congenital conditions (13.2%) mainly Down Syndrome Neoplasms (13.2%) mainly colon and breast cancer Circulatory diseases (11.8%) primarily ischaemic heart diseases External causes(5%) mainly choking on food
Respiratory Diseases Multiple risk factors include: swallowing difficulties reliance on others for assistance with meals mobility problems
Other factors impacting quality patient care Limited knowledge of the rights of the person Limited understanding of person s specific needs Faulty perceptions and attitudes such as: People with intellectual disability are unaware of what s going on around them They don t matter
Residents living in supported accommodation As they age and it is expected their health needs and admissions to hospital will increase Have unplanned admissions through the emergency department(ED) Have longer hospital stays and repeated admissions Disability Support Staff (DSW) provide 24 hour support to residents. They are not medically trained
Additional challenges in the hospital setting Communication barriers Complex behaviors/mental illness Fear and anxiety in unfamiliar environments Relevant information not being provided or getting lost Lack of understanding of person s specific needs
Often the barrier to the person is us It is important to listen to understand what the person is saying Our aim is to: Treat every person with dignity and respect Communicate with them as an individual Facilitate a barrier free environment for them
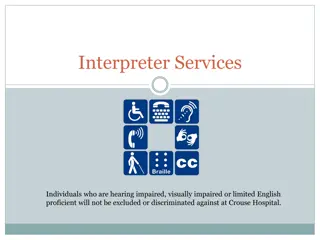
Communication Challenges Some residents are non-verbal and communicate through signs, gestures and behaviours Communication may not be straightforward, support may be needed to ensure their needs are met and that they are heard The person may use communication aids Do not assume that the person will have communication barriers because they have a disability, but they may.
Attitudes and Beliefs Our attitudes can change almost anything If your attitude towards the person in your care is positive then this will influence the way in which you care for the person.
Hospital are scary! Behaviours of concern may mean that the person: Has pain - unable to tell you. Has past negative experiences in hospital Is frightened - unfamiliar people or too busy or noisy environment Has a mental illness Does not understand what s going on around them Be experiencing all of the above
James Story James is a 47 year old man who lives in a group home James has an intellectual disability and is non verbal He communicates with signs and gestures James has autism.
James was discharged into the care of his parents. James was taken to ED. He was very agitated and tried to get out of the bed . The doctor was having difficulty taking bloods. When he was 17 James was staying at respite while his parents went on their first holiday since he was born They were informed that restraint was used to take blood. 5 people were needed to restrain James so bloods could be taken Lifelong Impact Taken to Emergency Home Ambulance 30 years later medical procedure that involves needles is still very traumatic. He was unwell so the DSW called 000 and asked for ambulance assistance. The DSW was unable to go to the hospital with him . James parents were contacted by the respite staff. . His parents are convinced that this trauma could have been avoided if he was supported differently in hospital all those years ago. . . It took them a few hours to return from holiday. James was very distressed when they arrived. 20 20
A2D Together Folder Front cover Contacts/photo Medication chart and Webster Pack TOP 5 tips for support Hospital Support Plan Mealtime Management Plan Other relevant plans to support the person in hospital It is important that this information stay with the person at all times
End of life plans - Authorised care plan or/and - Palliative care plan - In the front section of their folder - Highlighted on the cover page of the A2D Together Folder
Consent to medical treatment Medical Practitioners - legal and professional responsibility to obtain consent to treatments If patient unable to consent - seek consent from the patient s person responsible (The Guardianship Act 1887) Disability Support staff are not permitted to consent to medical treatment. Their role is to support the patient and provide the name of the person responsible A2D Together Folder
Treatment considered urgent and necessary Save patient s life Prevent serious damage to health Prevent or alleviate significant pain or distress No Consent is required
TOP 5 is designed to assist the hospital staff better understand the individual needs of the person developed by people who know the person well and include: any risks eg choking, pica interests, likes, dislikes, fears/ phobias, rituals/routines things that might trigger the person to become upset whilst in the hospital setting
Tips for communicating Read the TOP 5 and hospital support plan Address the person by their name Speak directly to the person (not support staff) Speak normally (no shouting) Make eye contact Allow personal space Use appropriate language Allow time to communicate/ don t rush the person Respect the person
Bills journey Bill was sent home arrived at 7am in a calm state. He had: - A2D folder - Follow up appointment - Discharge summary NO NEEDLES! Medical Officer READ A2D Folder and contacted Disability Staff at Group home Arrived unaccompanied to ED Paramedic gave A2D Folder to Triage nurse Fell at home- 2am Head wound & injured shoulder Home 7am Taken to Emergency Benefits & Savings for: Client Medical Staff Nursing/Allied Health staff Organisation Ambulance called Information shared joint decision made for best treatment Head wound Glued no needles No blood taken DSW gave Paramedics his A2D Folder . 27
What worked for Bill? He had his A2D Together Folder. It included: TOP5 Hospital Support plan Other relevant information Health staff read and used the A2D Together Folder, worked together with Disability Staff to provide safe, person centred care.
More Information A2D Together Website: www.a2d.healthcare Further education available e-HETI online for NSW Health staff about Disability & Carers Idmh e-learning UNSW Agency for Clinical Innovation (ACI) : The Essentials National Roadmap for Improving the Health of people with Intellectual Disability Content correct at time of development November 2021