Hemostasis and Clotting: Prevention of Blood Loss
Hemostasis refers to the prevention of blood loss by stopping bleeding from injured vessels. It involves vasoconstriction, platelet aggregation, and blood coagulation, working together to inhibit clot formation and dissolve clots once formed. This process is crucial for maintaining the integrity of the circulatory system and preventing excessive bleeding during injuries.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
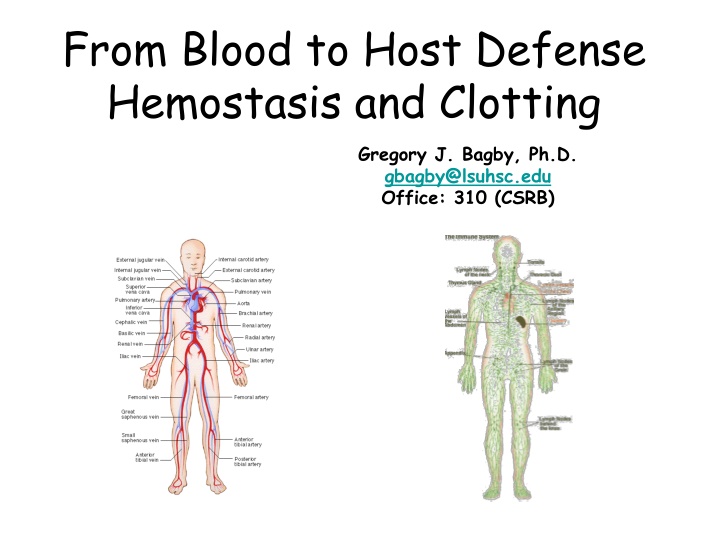
From Blood to Host Defense Hemostasis and Clotting Gregory J. Bagby, Ph.D. gbagby@lsuhsc.edu Office: 310 (CSRB)
From Blood to Host Defense Blood Components and function Hemostasis and clotting The host defense system General overview Innate immune system pathogen recognition inflammatory response Adaptive immune system Humoral immune system and antibodies Cell-mediated immune system
Definition Hemostasis is the prevention of blood loss by arresting of bleeding from injured vessels
Hemostasis and Its Control Most effective with small vessels. The greater intravascular pressure the harder it is to prevent blood loss. Hematoma - accumulation of blood in tissue. Three processes to decrease blood loss. Vasoconstriction Platelet aggregation Blood coagulation or clotting Steps to inhibit clot formation and dissolve clots once formed Anticlotting system Fibrinolytic system
Steps in Hemostasis following vessel injury: Vasoconstriction Only effective in the smallest of vessels. Injury leads to local contraction of vascular smooth muscle. Mechanism unclear endothelial cell disruption, mechanical stimulation, local mediators (EC, perivascular neurons) Constriction presses opposed endothelial surfaces together Contact induces stickiness between surfaces adhesion molecules bind/adhere Decreases blood flow to prolong contact time of damaged vessel with platelets
Steps in Hemostasis following Vessel Injury: Platelet Aggregation Plasma von Willebrand factor binds to collagen which binds to platelets Platelets degranulate to release mediators ADP and thromboxane A2 - amplifies platelet adherence and degranulation. Serotonin stimulates constriction Thromboplastin stimulates coagulation Plasma fibrinogen bridges between platelets (aggregation)
Inhibition of Platelet Aggregation Adjacent endothelial cells produce agents that inhibit platelet activation/aggregation and cause vasodilatation: 1. Prostacycyclin (PGI2) Inhibits platelet function 2. Nitric oxide - Vasodilator
Steps in Hemostasis following vessel injury: Coagulation Blood coagulation transformation of blood into a gel (clot or thrombus) Main ingredient a polymer of fibrin that forms a mesh Local response around a platelet plug Complex process involving sequential re-enforced activation of plasma factors (proteins) Key step in clotting pathway is production of the enzyme thrombin Thrombin cleaves fibrinogen to fibrin (soluble) which bind together to form loose mesh Thrombin activates Factor XIII which covalently cross-links fibrins to stabilize the fibrin network Thrombin activates clotting pathway leading to own production
The clotting pathway or cascade involves about 15 proteins. Thrombin plays directly initiates clot formation by catalyzing the conversion of fibrinogen to fibrin, and serving as a positive feedback modulator of the cascade.
Platelets & Calcium Important in Clot Formation Blood cells trapped in the fibrin meshwork, but not essential Clot possible in absence of cellular elements except platelets. Thrombin activates platelets in addition to vessel injury Activated platelets express receptors that bind several of the clotting factors Allows reactions to occur on the surface platelets Platelet factor (phospholipid) serves as a cofactor for clotting pathway reactions Calcium also required for several steps (always sufficient)
The Clotting Cascade from Injury to Thrombin Formation Two pathways leading to pro-thrombin to thrombin reaction Intrinsic pathway constituents all in the blood Extrinsic pathway cellular elements outside blood are needed Two pathways activated in sequence with thrombin serving as the link between them.
Clotting Cascade Intrinsic pathway Collagen activated Inactive to active proteases Cofactors (VIIIa & Va) Extrinsic pathway Cell-assoc Tissue Factor Thrombin produced by this pathway activates factors in the intrinsic pathway. Results in more thrombin to accelerate fibrin formation
Procoagulant Actions of Thrombin Cleaves fibrinogen to fibrin Activates clotting factors Factor XIII to cross-link fibrin Intrinsic pathway via factor XI Important co-factors VIII and V Stimulates platelet activation
Hemophilia Mostly genetic X-linked disorders seen primarily in men. Hemophilias Hemophilia A or classical hemophilia - Lack of factor VIII (~77% of cases). Hemophilia B - Lack of factor IX. Hemophilia C (both sexes) Lack of factor XI. Mild because IX (which is activated by XI) can also be activated by VII. Symptoms in life and disabling. Bleeds impair joint function. Treated by transfusions of plasma and injections of purified clotting factors (expensive to treat and inconvenient to the patient). Surgery, simple dental procedures - life-threatening. 14
Liver Plays Important Indirect Role in Clotting Site of clotting factor synthesis Vitamin K Bile salts produced by liver important vitamin K, a lipid soluble vitamin, absorption Vitamin K important for clotting factor synthesis Prothrombin Other clotting factors Liver failure results in sever bleeding problems
An Endogenous Anticlotting and Clot Lysing System Prevent, Limit or Remove Clots Endogenous anticlotting system - Factors that oppose and limit clot formation. The fibrinolytic system dissolves clots after they are formed. Anticlotting drugs Used to treat patients to decrease clotting or dissolve clots that inappropriately stop blood flow to important tissue (heart, brain).
Three Factors that Oppose Clot Formation Plasma tissue factor pathway inhibitor (TFPI) binds to and inhibits tissue factor-factor VIIa complexes to inhibit continuous production of factor Xa Extrinsic pathway only generates small amount of thrombin Thrombin binding to thrombomodulin on endothelial cells Inactivates thrombins clot-producing effects Bound thrombin binds to plasma protein C which inactivates Factors VIIIa and V Thrombin indirectly inactivates clotting Plasma antithrombin III Inactivates thrombin and other clotting factors Works via binding to heparin on endothelial cells Prevents spread of the clot to uninjured areas
Fibrinolytic System Removes Clots as Part of the Repair Process It s as complex as clotting with activators and inhibitors Plasminogen activators, important e.g. is t-Pa Plasminogen activators like Tissue Plasminogen Activator (t-PA) Plasminogen Plasmin Soluble Fibrin Fragments Fibrin Synthetic plasminogen activators can be used immediately after a stroke or heart attack to help dissolve clots and restore blood flow.
Anticlotting Roles of Endothelial Cells Barrier between blood and subendothelial extracellular matrix and cells inhibits platelet aggregation & formation of TF-VIIa complexes Synthesis of PGI2 and nitric oxide inhibits platelet activation and aggregation Secretes tissue factor pathway inhibitor inhibits TF- factor VIIa complexes to generate Xa Binds thrombin via thrombomodulin to activate protein C inactivates factors VIIIa and Va Display heparin on surface binds antithrombin III to inactive thrombin and other clotting factors Secretes tissue plasminogen factor catalyzes formation of plasmin to dissolve clots
Anticlotting and Thrombolytic Drugs Agents that depress the action of procoagulants Aspirin platelet cyclooxygenase inhibitor. Oral anticoagulants (Dicumarol) inhibits action of vitamin K required for synthesis of clotting factors by the liver. Heparin activates antithrombin III. Fibrinogen blockers - interfere with fibrinogen binding to platelets. Agents that dissolve clots (thrombolytic drugs) Recombinant t-PA Desmodus rotundus salivary plasmninogen activator (DSPA) Streptokinase