Health Information Management and Quality Programs Overview
This content provides expert advice on managing health information and quality through pay-for-performance programs. It covers types of quality measures, quality programs at national and Maryland level, financial impacts in Maryland, and performance periods. The information highlights the importance of collecting data, using quality measures effectively, and understanding the impact on reimbursement and penalties in healthcare.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
complex problems. EXPERT ADVICE. Health Information Management and Quality Pay- for-Performance Programs Kristen Geissler, MS, PT, CPHQ, MBA Managing Director, Berkeley Research Group May 6, 2016
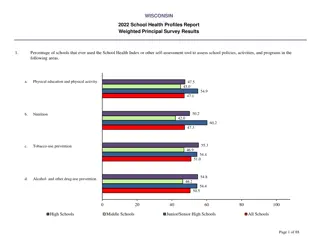
Types of Quality Measures Process Was a specific element of patient care provided? Evaluation of left ventricular function Outcome What happened with the patient? Mortality, Readmission, Complication Facility-reported Central line infection Concerns with hospitals using different methodologies and intensity of review Patient-reported HCAHPS Patient perception surveys 3
Types of Quality Measures Active Hospital must collect data from medical record and submit data Used for Core Measures & CDC/NHSN Healthcare-associated Infections Complex abstraction rules; time consuming Hospital has generous amount of time for re-reviews and validation Passive Claims-based Used for Mortality, Readmission, AHRQ Patient Safety Indicators (PSI), Hospital Acquired Conditions (HAC) Based strictly on coding/claims data Less opportunity for re-reviews and validation 4
Quality Programs National vs Maryland National (CMS) Maryland (HSCRC) Value-Based Purchasing (VBP) Quality-Based Reimbursement (QBR) Hospital Readmission Reduction Program (HRRP) Readmission Reduction Incentive Program (RRIP) Maryland Hospital Acquired Conditions (MHACs) (PPCs) Hospital Acquired Conditions (HAC) 5
Maryland Quality Financial Impact CMS Maryland (Inpt all-payer revenue) (Inpt Medicare revenue) VBP QBR Max Penalty 2% Max Reward variable Max Penalty 2% Max Reward 1% HAC MHAC Max Penalty 1% Max Reward 0 Max Penalty 3% Max Reward 1% HRRP RRIP Max Penalty 3% Max Reward 0 Max Penalty 2% Max Reward 1% Total Total Max Penalty 7%, but capped at 3.5% Max Penalty 6% Max Reward variable Max Reward 3% 6
Performance Periods FY2017 Impact CY2015 FY2018 Impact CY2016 Process, HCAHPS, HAI, Efficiency VBP (National) Mortality, PSI Oct 2013 June 2015 Oct 2014 Sept 2015 Oct 2014 June 2016 Oct 2015 Sept 2016 Process, HCAHPS, HAI QBR (Maryland) Mortality, PSI CY2015 July 2012 June 2015 July 2013 June 2016 CY2015 July 2013 June 2015 July 2014 June 2016 CY2014 & CY2015 CY2015 CY2016 HRRP (National) RRIP (Maryland) CY2016 PSI HAC (National) HAI CY2015 & CY2016 CY2016 MHAC (Maryland) 7
Quality Based Reimbursement (QBR) Measure Categories for FY2018 Patient Experience of Care HCAHPS Survey plus 3 Care Transition Measures Safety AHRQ Patient Safety Indicators (PSI) (suspended for FY2018) Healthcare Acquired Infections CLABSI Central line associated blood stream infection CAUTI Catheter associated urinary tract infection SSI Surgical site infection C Difficile Clostridium difficile MRSA Pregnancy Care PC-01 Elective Deliveries < 39 weeks Mortality Maryland In-Hospital Risk Adjusted Mortality 8
Quality Based Reimbursement (QBR) Domain Distribution FY2018 15% 35% Mortality Experience of Care Safety 50% 9
Quality Based Reimbursement (QBR) Mortality Domain Maryland-unique metric In-hospital, all-condition (~38 APR DRGs) mortality Measurement period: January December 2016 Base period: FY2015 Risk adjustments: Age Gender Admitting APR ROM (risk of mortality 1-4) Transfers in from another hospital Risk-adjusted survival rate will be measured the same as other QBR measures compared to a statewide threshold and benchmark Attainment and improvement component 10
Quality Based Reimbursement (QBR) Financial Impact Final score compared against a predetermined financial scale Up to 1% potential reward Up to 2% potential penalty 11
Readmission Reduction Incentive Program (RRIP) Inpatient, all-payer, all-cause readmissions within 30-days of an inpatient admission Adjusted for planned readmissions Inter-hospital readmissions are included (readmission to any hospital) Risk-adjusted using Discharge APR SOI APR DRG grouper v31 FY2017 impact measurement CY2015 performance compared to CY2013 performance 9.3% improvement required to achieve a reward of up to 1% Improvement of less than 9.3% or erosion in risk-adjusted readmission performance results in penalty of up to 2% HSCRC is currently evaluating potential changes to FY2017 and FY2018 programs 12
National HRRP Readmissions FY18 Readmissions Measures 3% Maximum At Risk Medicare Revenue 30-day All-Cause Readmissions After Initial Admission for: Heart Failure Pneumonia Acute Myocardial Infarction COPD Exacerbation Total Hip/Total Knee Replacement CABG 13
Maryland Hospital Acquired Conditions (MHAC) 65 Potentially Preventable Complications 59 scored in CY2016 Two Tiers Tier 1 100% weight Tier 2 50% weight Risk adjusted using Admitting SOI Statewide improvement target CY2016 compared to FY2015 6% improvement in total observed to expected ratio 14
Maryland Hospital Acquired Conditions (MHAC) Financial Impact Statewide improvement target of 6% met 1% potential penalty 1% potential reward Statewide improvement target of 6% not met 3% potential penalty No potential for reward 15
National/CMS HAC Domains Hospitals in the bottom quartile nationally will have a 1% penalty Domain 1 Domain 2 15% 85% PSI-90 Patient Safety for Selected Indicators Composite CLABSI Pressure ulcer rate (PSI 3) CAUTI Iatrogenic pneumothorax rate (PSI 6) Added for FY16 Central venous catheter related blood stream infection rate (PSI 7) Surgical site infection (SSI) colon surgery and abdominal hysterectomy Postoperative hip fracture rate (PSI 8) Added for FY17 Post op PE or DVT rate (PSI 12) MRSA infection Postoperative sepsis rate (PSI 13) C diff infection Postoperative wound dehiscence rate (PSI 14) Accidental puncture or laceration (PSI 15) 16
Maryland Hospital Quality Programs Clinical Process Patient Perception (HCAHPS) Outcomes/Patient Safety Quality Based Reimbursement (QBR) Readmission Reduction Incentive Program (RRIP) 30-day, all-cause Readmission All conditions 3M Potentially Preventable Complications 65 complications (59 scored in 2016) Maryland Hospital Acquired Conditions (HAC) 17
Maryland Hospital Quality Programs Clinical Process Patient Perception (HCAHPS) Outcomes/Patient Safety Quality Based Reimbursement (QBR) Process/ Active Patient reported Outcome/ Passive Readmission Reduction Incentive Program (RRIP) 30-day, all-cause Readmission All conditions 3M Potentially Preventable Complications 65 complications (59 scored in 2016) Maryland Hospital Acquired Conditions (HAC) 18
Maryland Quality Programs Clinical Process Patient Perception (HCAHPS) Outcomes/Patient Safety Value Based Purchasing (VBP) (QBR) Quality Based Reimbursement Process/ Active Patient reported Outcome/ Passive Hospital Readmission Reduction Program (HRRP) Readmission Reduction Incentive Program (RRIP) 30-day, all-cause Readmission All Conditions Outcome/ Passive Hospital Acquired Conditions (HAC) 3M Potentially Preventable Complications 65 complications (59 scored in 2016) Maryland Hospital Acquired Conditions (HAC) 19
CMS Hospital Quality Programs Clinical Process Patient Perception (HCAHPS) Outcomes/Patient Safety Value Based Purchasing (VBP) (QBR) Quality Based Reimbursement Process/ Active Patient reported Outcome/ Passive Readmission Reduction Incentive Hospital Readmission Reduction Program (HRRP) Program (RRIP) 30-day, all-cause Readmission All Conditions Outcome/ Passive Hospital Acquired Conditions (HAC) 3M Potentially Preventable Complications 65 complications (59 scored in 2016) Maryland Hospital Acquired Conditions (HAC) Outcome/ Passive 20
Maryland Quality Financial Impact CMS Maryland (Inpt all-payer revenue) (Inpt Medicare revenue) VBP QBR Max Penalty 2% Max Reward variable Max Penalty 2% Max Reward 1% HAC MHAC Max Penalty 1% Max Reward 0 Max Penalty 3% Max Reward 1% HRRP RRIP Max Penalty 3% Max Reward 0 Max Penalty 2% Max Reward 1% Total Total Max Penalty 7%, but capped at 3.5% Max Penalty 6% Max Reward variable Max Reward 3% 21
Performance Periods FY2017 Impact CY2015 FY2018 Impact CY2016 Process, HCAHPS, HAI, Efficiency VBP (National) Mortality, PSI Oct 2013 June 2015 Oct 2014 Sept 2015 Oct 2014 June 2016 Oct 2015 Sept 2016 Process, HCAHPS, HAI QBR (Maryland) Mortality, PSI CY2015 July 2012 June 2015 July 2013 June 2016 CY2015 July 2013 June 2015 July 2014 June 2016 CY2014 & CY2015 CY2015 CY2016 HRRP (National) RRIP (Maryland) CY2016 PSI HAC (National) HAI CY2015 & CY2016 CY2016 MHAC (Maryland) 22
Strategy for Success HIM/Docu mentation Nursing Finance Medical Staff Quality/PI 23
Improvement Strategies Oversight Education Data Analysis Medical Record Review 24
Improvement Strategies Education Leadership Financial impact Resources Front-line staff Coding and documentation professionals Methodology and opportunities Medical staff Documentation guidelines Clinical definitions 25
Improvement Strategies Data Analysis Improvement Opportunities Service/product line Physician MS-DRG Trends Present on admission Diagnoses Service line and physician 26
Improvement Strategies Record Review Timing Concurrent Retrospective Type Coding Clinical Documentation Quality Medical staff 27
CDI Benefit in Maryland Maryland no longer reimburses hospital care with a fee- for-service reimbursement, and instead uses a fixed- revenue budget (called GBR Global Budget Revenue) Value of a CDI program will be to perform positively on Quality, Efficiency and Market Share measurements in order to maintain the hospital s current revenue base and Maryland has close to 9% of total inpatient revenue at risk in the various quality and revenue adjustment methodologies 28
CDI Impact in Maryland Maryland Hospital Acquired Conditions (MHAC) Impact on actual MHAC assignment Risk adjustment using admitting SOI Readmission Reduction Incentive Program (RRIP) Risk adjustment using final SOI Mortality a component of Quality Based Reimbursement (QBR) Risk adjusted using admitting ROM Market Shift Adjustment Risk adjustment using final SOI Efficiency Measure under development 29
CDI Impact in Maryland, Continued Patient Safety Indicators (AHRQ PSI) a component of QBR and used in many national public report cards Impact on actual PSI assignment Risk adjusted using a unique APR DRG adjustment factor Other impact nature of admission and admission source Potentially Avoidable Utilization (PAU) Readmissions Risk adjusted using final SOI Prevention Quality Indicators (PQI) Determined based on principal diagnosis Other impact admission source 30
QBR/VBP Strategy Clinical Process Confirmation of principal diagnosis Core measures documentation requirements Outcomes Mortality risk adjustment AHRQ Patient Safety Indicators (PSI) Coding of complication Present on admission Exclusions Risk adjustment 31
RRIP/HRRP Strategy Risk adjustment Documenting and coding all diagnoses Acuity and specificity of diagnoses Inpatient and outpatient 32
MHAC/HAC Strategy Appropriate documentation and coding of complication Clinical indicator support Condition ruled out Contradictory information Appropriate assignment of present on admission indicator Signs and symptoms on admission Timing of labs and diagnostic tests 33
Present on Admission Definitions Defined by the Inpatient Coding Guidelines as present at the time the order for inpatient admission occurs conditions that develop during an outpatient encounter, including: emergency department observation outpatient surgery are considered to be present on admission Timing of documentation DOES NOT MATTER Physician may document that a diagnosis was present on admission at any time, including discharge summary or post- discharge query 34
Present on Admission Indicators Present on admission Y condition was present on admission N condition was NOT present on admission W provider is unable to clinically determine whether condition was present on admission or not U documentation is insufficient to determine if condition is present on admission E diagnosis is exempt from POA reporting W is treated the same as Y by CMS 35
Thank you! Kristen Geissler, MS, PT, CPHQ, MBA Managing Director Berkeley Research Group, LLC M 443.845.3641 kgeissler@thinkbrg.com 36