Enhancing Health Interventions for Better Access and Quality
Considerations for health interventions include addressing barriers such as availability, accessibility, and affordability. Principles emphasize free essential health services during crises, with a focus on reducing financial barriers. Financing approaches aim to ensure qualified health service providers are accessible and affordable, protecting against catastrophic health expenditures. Various response options, including cash and voucher assistance, play a crucial role in improving access to health services in humanitarian settings. Evidence shows that cash assistance contributes positively to health outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Three barriers we have to consider when thinking about health interventions and ensuring quality of health services: Health Assistance During Crises Availability Accessibility and, Affordability 2
Principles: Essential health services during a humanitarian crisis should be provided free of charge at the point of delivery UHC Health Assistance During Crises Addressing health needs are different and unpredictable In reality: people still have direct as well as indirect health expenditures 3
Foundation for all financing approaches: Availability of health services from qualified providers Health Financing Accessibility and affordability reducing financial barriers to accessing health services, and protection against catastrophic health expenditures 4
Supply Side Response Options Coverage under a health insurance fund Purchasing services from providers to deliver prioritised health services (based on inputs, outputs, and performance) Health Equity Funds Health Financing Demand Side Response Options Vouchers for health services Cash to reimburse costs for services, and/or for indirect costs Using part of MPC for remaining health expenditures (including medication, transport, etc.) Important that we that we don t inadvertently support an OOP culture which will undermine equitable financing for universal health coverage. Therefore these two finance options should go hand in hand. 5
Cash & Voucher Assistance (CVA) can be useful to improve access to and utilisation of health services in humanitarian settings, by reducing direct and indirect financial barriers and/or by incentivising the use of free preventive services. When health services are available with adequate capacity and quality but user fees are applied, the preferred response option is through provider payment mechanisms, with CTP to be considered complementary to such supply side health financing strategies, and not aim to replace these. Using CVA for Health outcomes CVA cannot solve supply side challenges such as insufficient health facilities or lack of health care workers
Evidence of cash assistance to contribute to health outcomes in humanitarian settings is slowly emerging, particularly on reducing financial barriers to accessing health services. No indication that the evidence from development programs would not apply to humanitarian settings, though adaptation required of implementation and risk management Current Evidence shows that CVA for health projects with the highest impact are those combined with other health interventions, particularly if it incentivizes policy reform. Evidence on CVA and Health CVA can effectively reduce the financial cost to the beneficiary of accessing services. CVA can work as incentives for behaviour change and increase service utilisation (vaccination, food diet, completion of treatment) CVA (vouchers) can also create competition to ensure providers provide quality services A gap remains for well-designed studies comparing different response options and implementation, for optimal effectiveness of cash transfers on health utilization and outcomes 7
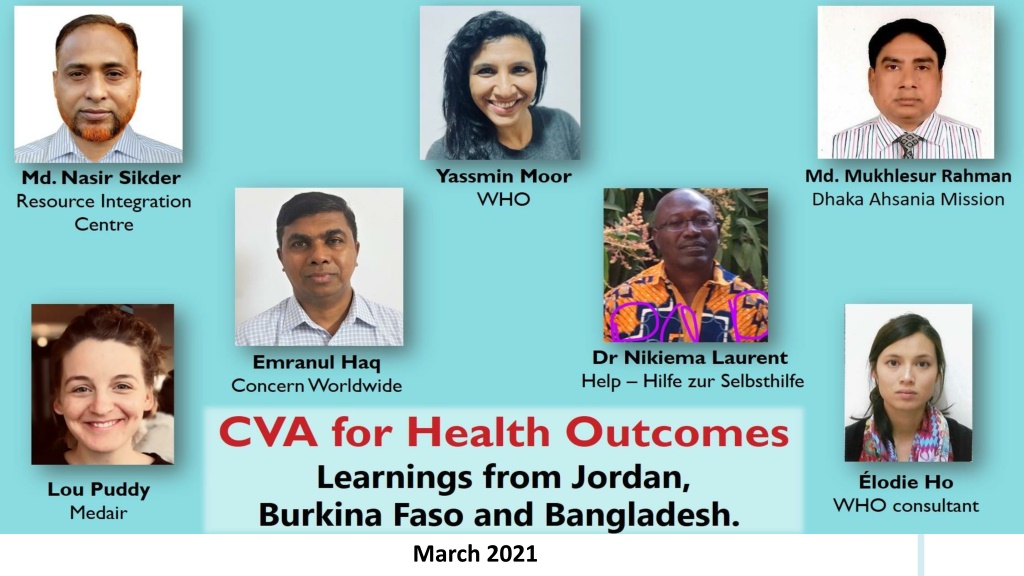
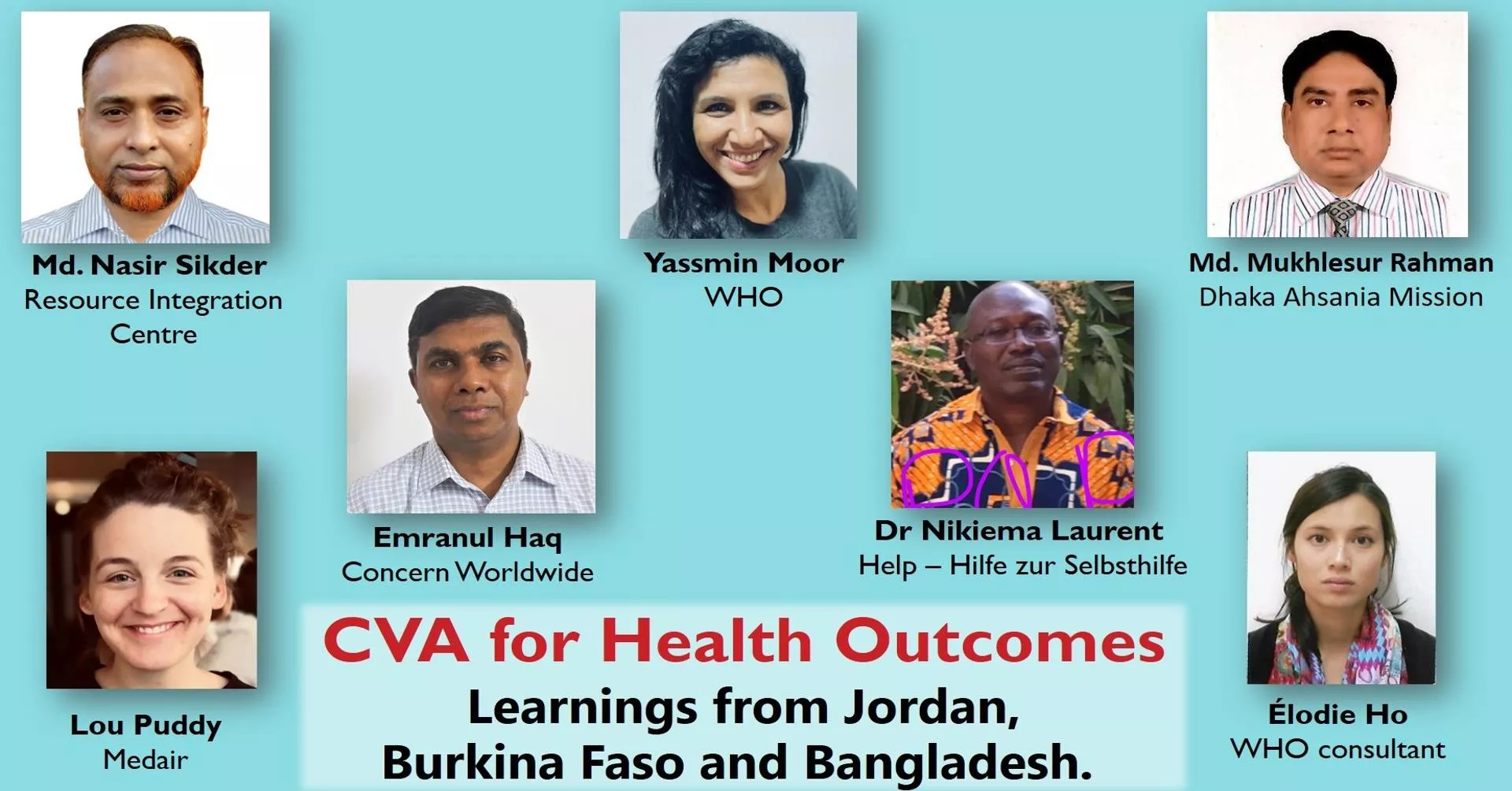
Three Case Studies from Jordan, Bangladesh and Burkina Faso 8
A Case Study from Jordan: Cash & Voucher Assistance A Case Study from Jordan: Cash & Voucher Assistance for Health for Health Syrian refugees were incurring high health related costs. The OOP expenditures was also a barrier in accessing essential health services. Purchasing of services by international partners would increase the budget requirements because organizations would pay the international rate. The next response option was then to provide unconditional cash transfers to compensate them for their user fees and indirect costs related to accessing health services UCT linked with a health need targeting pregnant women unable to cover delivery costs CCT used to incentive access to health services such as ANC, NCD s Reimbursement of priority health service from a pooled fund and based on receipts of an acute health need 6,892 refugees targeted. 9
Health and Nutrition Vouchers for Marginalized Urban Health and Nutrition Vouchers for Marginalized Urban Extreme Poor in Bangladesh Extreme Poor in Bangladesh Three pilots by three partner organizations targeting 10 municipalities across Bangladesh Concern with Sajida Foundation Dhaka Ahsania Mission (DAM) with Christian Aid Resource Integration Center (RIC) High user fees and distance barrier to accessing services and is a major reason why people postpone or forego healthcare despite increased health needs linked to user fees as well as other barriers related to accessing health services. Vouchers to address the health gaps for the urban poor The total number of vouchers that were distributed in 10 municipalities was around 80,000, covering 337,000 persons 10
Case Study from Burkina Faso: Cash Transfers for Transport to Case Study from Burkina Faso: Cash Transfers for Transport to Health Centers and Malnutrition Treatment Centers Health Centers and Malnutrition Treatment Centers Cost of crossing m,nseasonal lakes created a financial obstacle to accessing nutrition centers Cash for adults accompanying children to receive treatment for mal-nutrition 23 children targeted Reduced financial barriers to accessing the nutrition centers. There was an increase in attendance of these center, and a and a reduction in the mortality rate for cases of Severe Acute Malnutrition (SAM) during the cash distribution period compared with 2018. 11