Eating Disorders in Schools: A Comprehensive Guide
This guide sheds light on the alarming increase in eating disorder referrals since March 2020, especially among young individuals. It explores the impact of lockdown on behaviors, provides insights into diagnostic features, behavioral indicators, and discusses ARFID. Early intervention is crucial for better outcomes. Referral to the CYP ED Team for every young person under 19 with a probable eating disorder is essential to ensure timely medical attention and support.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Eating Disorders in Schools A Guide
Incidence current picture Significant regional, national and local increases in numbers of young people and adults being referred to ED services since March 2020. Suffolk ED Referrals (Under 19s) 60 50 40 30 20 10 0 Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec 2019 2020
Young peoples experience Too much time to think No distractions Limited activity Disruption of normal patterns of eating, shopping, meal prep Everyone together/apart for meals Extended and significant use of social media Impact of lockdown on general mood, anxiety, self esteem, isolation Dieting behaviours Changes in exercise behaviours
Behavioural indicators Early intervention is associated with better outcome Behavioural indicators of an eating disorder include: Reluctance to discuss concerns (when concern raised by parent or school) o Resisting weighing o Evasiveness o Getting angry or distressed when asked about eating problems o Increased isolation o Changes to eating behaviours o
Diagnostic features of an eating disorder (anorexia nervosa, bulimia nervosa) Restriction of energy intake Severe weight loss and/ or significantly low weight for age Intense fear of weight gain Disturbed body image, or lack of recognition of seriousness of weight loss Compensatory behaviours: eg self-induced vomiting, excessive exercise, laxative use Symptoms of low weight: eg feeling cold, dizziness, secondary amenorrhoea in girls In some patients: recurrent bingeing (lack of control over eating)
ARFID Some people present with very low weight, often long- standing, due to lack of appetite, sensory sensitivity, or anxiety Avoidant/ Restrictive Food Intake Disorder They do not have a fear of weight gain, nor disturbed body image. There is no dedicated service for these patients in Suffolk currently, but they may require advice from paediatrics and/or mental health services.
Refer to CYP ED Team every young person under 19 with probable eating disorder. Referral Members of school community can refer via Emotional Wellbeing Hub Refer urgently for medical attention - : Rapid weight loss with BMI under 0.4thcentile Lost more than 1kg/ week for >2 weeks Heart rate under 40 bpm Blood pressure under 85/40 Ecg abnormality Severe dehydration Temperature < 35.5 C
Include: weight, height, pulse, blood pressure, temperature How to refer to CYP ED Team Any previous records of weight or height even if years previously Behavioural concerns/changes Concerns about overall mental wellbeing Safeguarding concerns Referral Form (via Children and Young People s Emotional Wellbeing Hub) is on the SuffolkInfoLink website. Professionals, parents, carers and young people can also contact the Hub on: 0345 600 2090, Monday to Friday 8am 7.30pm for consultation or advice
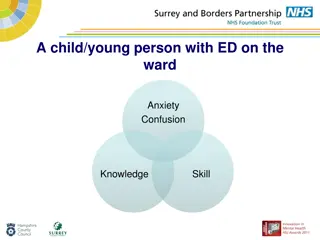
School support Vast majority of young people with an ED will maintain full school attendance throughout the course of their treatment/illness May require modifications to timetable, eg changes to PE Will require time to attend treatment appointments May require modifications to exam programming May require support around mealtimes-environment, other immediate support Maintaining friendships How will I keep up Impact of physical and psychological state on ability to study-energy required to compensate for this can be overwhelming and v. stressful
WHAT INFORMATION TO GIVE TO YOUNG PERSON AND PARENT ? The parent (or young person) will be contacted by eating disorder team by telephone, usually within 1-2 working days, for a discussion. Assessments will usually be carried out within 7 days if urgent, or 28 days if routine. The YP will be seen on their own, as well as with a parent, unless they prefer not to do so Treatment is non-judgemental, closely involving parents in early stages; includes regular physical checks; use of medication is not routine. Useful websites: Suffolkinfolink, MindEd, Young Minds, BEAT