Eating Disorders: Insights for Dietitians
Eating disorders are complex neurobiological conditions that are not merely about control or weight management. These disorders can affect individuals of all genders, body sizes, and socioeconomic backgrounds. Dietitians play a crucial role in identifying, assessing, and treating eating disorders, as well as in creating environments that support healthy relationships with food. Knowing the types of eating disorders, their etiology, and effective screening methods are essential for providing appropriate care and prevention strategies.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Eating Disorders: What Dietitians should know and considerations for prevention in our own practices LAURIE FORTLAGE, MS, RD C.S. MOTT CHILDREN S HOSPITAL
https://create.kahoot.it/share/eating-disorders-myths-vs- facts/3f5defe1-71bb-4daf-8439-9f5014b77901
Objectives Eating Disorder Diagnoses Identifying Eating Disorders in your office Assessment tools Treatment Promoting environments and Acting in ways that do not promote disordered eating or thoughts about eating
What is an Eating Disorder? Eating Disorders are neurobiological disorders rooted in the brain causing medical and psychological issues They are NOT a choice and not simply about control or weight management Genetics, Environment, Temperament all play a role Experienced by all genders, body sizes, SES
Types of Eating Disorders Anorexia Nervosa (AN) Restriction of energy intake; Body image disturbance Bulimia Nervosa (BN) Recurrent binge eating episodes and compensatory behaviors that are meant to prevent weight gain Binge Eating Disorder (BED) Recurring and persistent episodes of binge eating with the absence of regular compensatory behaviors Other Specified Eating or Feeding Disorders (OSFED) Symptoms of an eating disorder but don t meet full criteria Avoidant Restrictive Food Intake Disorder (ARFID) Limitations on the amount or types of food intake; without distress about body shape or size or fears of fatness
Etiology of EDs Impossible to know the exact cause/causes Often referred to as the Perfect Storm of: Environment Genetics Temperament Stress activates this combination of events Individuals manage the stress by controlling food intake Many have underlying anxiety disorders Can t treat the anxiety disorder until the person is nourished
Check your Assumptions ANY client can have or could develop an eating disorder Don t assume that by looking at someone you will know. EDs are rarely recognized by how someone looks Initially assess in your usual manner, and keep an eating disorder in the back of your mind EDs can t exist if they can t keep it a secret Do no harm
How does a client with an eating disorder show up in your practice? GI disturbances IBS, food sensitivities, stomach pain, bloating Athletes New Vegetarians/ Vegans Lengthy or complicated dieting histories DM, Type 1 (diabulimia) Picky Eating ; Autism Spectrum; ARFID Bariatric Surgery Patients Polycystic Ovarian Syndrome
AN Traits Perfectionism Personal self-imposed standards Anxiety OCD tendencies Rigid thinking Risk avoidant Experiential avoidant Rule followers
BN Traits Impulsive Compulsive Novelty Seeking More likely to have a chaotic environment
What to look for. Are they seeking weight loss? Weight history, desired weight Do they count calories? What happens if they eat more than their goal for the day/meal? Do they ever feel out of control around food? Are there foods they won t eat because of a belief or rule? Is there flexibility around this? Do they save their calories for later in the day? Will they eat food they haven t prepared or don t know the ingredients and/or calories of? Do they avoid events with food or eating with other people?
What to look for.. Food rituals; food rigidity Do they ever sneak food? Have they lied about having something or not having something? Do they feel the need to compensate for the calories they ate? Are they weighing themselves? How often are they weighing themselves? How does weight impact their food choices, mood for the rest of the day? Do they ever feel guilty or shameful during or after eating? What happens if they eat more than they wanted?
Screening tools for Eating Disorders Eating Attitudes Test (EAT-26) EDGE Symptom Survey BED Screening Female Athlete Screening Tool (FAST) SCOFF Eating Disorder Screening Tool for Primary Care (ESP)
Eating Attitude Test (EAT 26) https://www.seattlechildrens.org/globalassets/documents/healthca re-professionals/pal/ratings/eat-26-rating-scale.pdf
Binge Eating Disorder Screener (BEDS-7) https://www.vyvansepro.com/documents/Adult-Binge-Eating- Disorder-Patient-Screener.pdf
Female Athlete Screening Tool (FAST) https://uhs.nd.edu/assets/165496/female_athlete_screening_tool_20 11_12.pdf
SCOFF Questionnaire The SCOFF questions* Do you make yourself Sick because you feel uncomfortably full? Do you worry you have lost Control over how much you eat? Have you recently lost more than One stone (14 lbs) in a 3 month period? Do you believe yourself to be Fat when others say you are too thin? W Would you say that Food dominates your life? *One point for every yes ; a score of 2 indicates a likely case of anorexia nervosa or bulimia Morgan, Reid, Lacey, The SCOFF questionnaire: assessment of a new screening tool for eating disorders, British Medical Journal (BMJ), 319(7223): 1467 1468, December, 1999.
Eating Disorder Screening Tool for Primary Care (ESP) Are you satisfied with your eating patterns? (A no to this question was classified as an abnormal response). Do you ever eat in secret? (A yes to this and all other questions was classified as an abnormal response). Does your weight affect the way you feel about yourself? Have any members of your family suffered with an eating disorder? Do you currently suffer with or have you ever suffered in the past with an eating disorder? Cotton, Ball, Robinson, Four Simple Questions Can Help Screen for Eating Disorders Journal of General Internal Medicine,18(1): 53 56, January, 2003.
Assessment Tools Health history, family history Lifestyle assessment including social impact of eating disorder Review of lab results to assess nutrient status Food intake assessment and analysis Meal Planning Metabolic assessment (RMR) and estimated needs analysis
Consequences of Undernutrition Medical Instability Vital Sign Abnormalities Adaptive, compensatory response to malnutrition Hibernation Mode - hypothermia, hypotension, hypoglycemia
Consequences of Undernutrition Bradycardia <60 bpm Heart muscle atrophy Severe Sinus Bradycardia <50 bpm Often <45 while sleeping Glucose < 60 high risk Low glucose is a result of depletion of glycogen scores Cold extremities Edema Lanugo Hair Loss
Consequences of Undernutrition Amenorrhea Not always present even in critically ill clients Osteopenia With AN body loses bone secondary to low estrogen Weight restoration is the gold standard Birth control pill are not helpful Keep Vit D levels > 30 ng/UL
Consequences of Undernutrition Gastroparesis Emptying 5x slower Decreased peristalsis Early fullness, bloating, gassiness, nausea Frequent meals Challenge safe versus dense foods Brain Loss of gray matter Serotonin and dopamine receptors impaired (pleasure/pain/reward)
4 Cs of Malnutrition Cold Crabby Constipation Poor Circulation
Anorexia Nervosa Initial goal: adequate calories; dense foods are predictive of recovery outcomes Normalized and balanced eating will come in time Meet them where they are *Full weight restoration* 90% IBW- about 50% relapse % body fat better predictor than BMI/Weight Intuitive Eating---takes time
Anorexia Nervosa Extremely high calorie need Require more calories to maintain the rate of weight gain Post weight restoration, these clients require more calories to maintain their weight Hyper-metabolism usually lasts 3 to 6 months, but can last up to a year after weight restoration
Bulimia Nervosa Recurrent binge episodes Recurrent use of inappropriate behaviors to prevent weight gain Both B/P occur on average, >1/week for 3 months Self-evaluation focused on weight/shape Does not meet criteria for Anorexia
Bulimia Nervosa Initial goal is to stop the purging cycle Often 5 pound weight gain once purging stops. Fluid shifts Regular meals and snacks Need satisfying foods: fat Find the sweet spot: not too hungry/not too full
Binge Eating Disorder Reoccurring episodes of eating large amounts of food Feelings of loss of control during binge episode, as well as marked distress Binge episodes occur on average >1x/week for 3 months
Binge Eating Disorder Assess timing of food intake Regular meals and snacks Mindful eating with focus on food Structure areas for eating Pacing Weight loss is not the primary goal leads to shame and keeps people in disordered eating patterns which increases the change of binging
What to do about Weights The weight of the client is not the only issue or even the main issue Crucial to develop trust Set up plan ahead of time with client Clients who should always be weighed: AN, laxative abuse, purging, just out of treatment center
Determining Expected Body Weight Set at least a 5 pound range understanding this may change along the way Growth charts Weight history When do behaviors and thoughts begin to diminish? Don t aim too low
Working with Clients Patients are hesitant to trust Secretive disorder Has been the driving force of their life You won t automatically be seen as an ally even if they initiated the appointment There is a paradox of not wanting to give up the eating disorder and also not wanting to work with someone the eating disorder can fool They want to know you re on their side while still challenging their eating disorder thoughts and behaviors You cannot work on weight loss and recovery from an eating disorder at the same time Separate the eating disorder from the person Eating disorder will behave in ways the person client wouldn t Feel shameful of their eating disorder behaviors
Working with Clients Pay attention to your own assumptions Be neutral until you know their reaction Know what matters to your patients you can use this to make challenges relevant Learn to sit in silence with your clients Listen to what s not being said Learn to ask questions differently (sometimes normalizing ED behaviors so they know you won t be shocked/judge them) Don t jump in and try to fix things Meet them where they are let them be involved in decision making while also understanding what s not negotiable Actions follow thoughts
Create a Safe Environment for your Clients Humor, kindness, compassion and empathy Tough fairness Safe environment for client to show frustration and anger Environment to share and process the relationship with the eating disorder and support them to use alternative behaviors to cope Explore and understand maladaptive thinking patterns that are directed at the behaviors and understanding the disease Don t be afraid of the client.
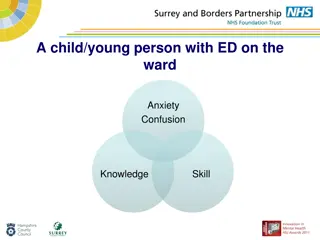
Treatment Team We cannot work with these clients alone Multi-disciplinary team of Therapist, Physician, Psychiatrist if needed Ideally the team should be specialist in eating disorders Obtain release of information to speak to all treatment team members Talk with clients ahead of time about talking with parents, care takers, spouses
9 Truths about Eating Disorders #1: Many people with eating disorders look healthy, yet may be extremely ill. #2: Families are not to blame, and can be the patients and providers best allies in treatment. #3: An eating disorder diagnosis is a health crisis that disrupts personal and family functioning. #4: Eating disorders are not choices, but serious biologically influenced illnesses. #5: Eating disorders affect people of all genders, ages, races, ethnicities, body shapes and weights, sexual orientations, and socioeconomic statuses. #6: Eating disorders carry an increased risk for both suicide and medical complications. #7: Genes and environment play important roles in the development of eating disorders. #8: Genes alone do not predict who will develop eating disorders. #9: Full recovery from an eating disorder is possible. Early detection and intervention are important. Produced in collaboration with Dr. Cynthia Bulik, PhD, FAED and the Academy for Eating Disorders, along with other major eating disorder organizations.
Prevention of eating disorders Patient centered care Think about the language and terms that we use Broaden the focus; weight is not a behavior we can change Focus on the person we are all unique All weight loss is not good weight loss Changing a client s food intake or restriction removes a coping mechanism. Be prepared to help find alternatives and/or work closely with the client s team so that someone is supporting them