Dissociative Disorders
Dissociative disorders involve a disconnection in consciousness, memory, perception, emotions, and identity. Symptoms range from depersonalization to amnesia, occurring on a continuum from daydreaming to chronic experiences. Treatment options and criteria for diagnosis are essential in managing these conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Dissociative Disorders David RM Trotter, PhD Associate Professor Departments of Family Medicine and Medical Education
Objectives By the end of this presentation, you should be able to: Discuss dissociation from a clinical and non-clinical perspective Review the epidemiology of Dissociative Disorders Describe the criteria for the various Dissociative Disorders Outline common treatments for Dissociative Disorders
What is Dissociation??? Dissociation is an experience in which there is a discontinuity in conscious awareness. This occurs when there is a disconnection in the usually integrated functions of consciousness, memory, perception, emotions, actions, identity, body representation, and/or motor control.
Common Dissociative Experiences Depersonalization: Experiences of unreality, detachment, or being an outside observer with respect to one s thoughts, feelings, sensations, body, or actions (e.g. perceptual alteration, distorted sense of time, unreal or absent self, emotional and/or physical numbing) Derealization: Experiences of unreality or detachment with respect to surroundings (e.g. individual or objects are experience as unreal, dreamlike, foggy, lifeless, or visually distorted) Dissociative Amnesia: Inability to recall important personal information in a way that cannot be explained by ordinary forgetting Identify Confusion or Alteration: Confusion: Confusion about who one is. For example, they may at times enjoy activities (e.g. drugs, alcohol, recklessness) that at other times they find repugnant. Alteration: The shifting of personality states
Positive and Negative Dissociative Symptoms Positive: Addition of an experience not typically there E.g. fragmentation of identity, depersonalization, derealization Negative: Lack of a typical experience E.g. amnesia NOTE: Think of this in the same way you think of positive and negative psychotic symptoms
Dissociation Occurs on a Continuum: Common Dissociation Daydreaming Being so absorbed in something (e.g. book/movie) that you are not aware of what is happing around you Feeling detached for your body in some way Loosing track of time Feeling emotionally numb
Dissociation Occurs on a Continuum: Less Common Dissociation Chronic Derealization and/or Depersonalization Amnesia for specific events, types of events, or important personal information The presents of more than one personality state
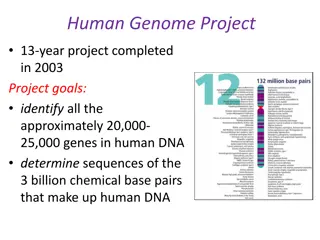
Causes for Severe Forms of Dissociation Causes assumed to be largely environmental and genetic A history of trauma is very common among individuals with dissociative disorders. This may include ACEs (e.g. abuse, neglect) or other intolerable/overwhelming experiences. Dissociation during a traumatic event predicts likelihood of dissociation occurring later. Remember, dissociation during a traumatic event is acutely adaptive. However, it may become disrupted later.
What is the primary function of Dissociation? Defense/Coping Mechanism
Dissociative Disorders Dissociative Identity Disorder (Previously Multiple Personality Disorder) Dissociative Amnesia Depersonalization/Derealization Disorder Other/Unspecified Dissociative Disorder
Dissociative Identity Disorder A. Disruption of identity characterized by two or more distinct personality states, which may be described in some cultures as an experience of possession. The disruption in identity involves remarked discontinuity in senses of self and sense of agency, accompanied by related alterations in affect, behaviors, consciousness, memory, perception, cognition and/or sensory-motor functioning. These signs and symptoms may be observed by others or reported by the individual. B. Recurrent gaps in the recall of everyday events, important personal information, and /or traumatic evens that are inconsistent with ordinary forgetting. C. The symptoms cause distress or impairment D. The disturbance is not a normal part of a broadly accepted cultural or religious practice. NOTE: In children, the symptoms are not better explained by imaginary playmates or other fantasy play E. Symptoms are not attributable to the psychological effects of a substance or another medical condition
Dissociative Identity Disorder A. Prevalence (12-month): 1.5% in the general population A. Male 1.6% B. Female 1.4% B. Often comorbid with other issues including depressive, anxiety, substance, self-injury, non-epileptic seizure disorders C. Developmental Couse A. Often associated with childhood trauma (about 90%) B. Decompensation often associated with a trigger: removal from traumatic situation, children reaching same age as they were when abuse began/occurred, later traumatic events (e.g. care accident), death or illness of abuser D. 70% of outpatients with DID have attempted suicide in the past
Dissociative Identity Disorder A. Differential Diagnosis A. Major Depressive Disorder B. Bipolar Disorders C. PTSD D. Psychotic Disorders E. Substance/Medication-induced disorders F. Personality Disorders G. Conversion Disorder H. Seizure Disorders I. Factitious Disorder and Malingering
Dissociative Identity Disorder Image result for sybil multiple personality
Dissociative Amnesia A. An inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting. NOTE: Dissociative amnesia most often consists of localized or selective amnesia for a specific event or events; or generalized amnesia for identify and life history B. The symptoms cause distress or impairment C. The disturbance is not attributable to use of a substance or another medical condition D. The disturbance is not attributable to another dissociative disorder With Dissociative Fugue: Apparently purposeful travel or bewildered wandering that is associated with amnesia for identity or for another important autobiographical information
Dissociative Amnesia Diagnostic Features Lack of memories is not a function of organic (i.e. neurological damage or toxicity) problems. Localized Amnesia: Failure to remember events that happened during a specific time frame Selective Amnesia: Failure to remember some, but not all, or events that happened during a time frame Generalized Amnesia: A failure to remember ALL one s life history (very rare). Often associated with dissociative fugue.
Dissociative Amnesia Prevalence (12-month): 1.8% Male: 1.0% Female: 2.6% Developmental Course: Trauma history is very common Individual is often unaware of the amnesia Onset of amnesia post trauma can be hours, days, or longer Amnesia can last decades After amnesia remits there is often significant depression and anxiety
Dissociative Amnesia Suicide Risk: This risk is high among those with dissociative amnesia, especially if amnesia remits suddenly. Differential Diagnosis: DID PTSD Neurocognitive Disorders Substance-related Disorders TBI Seizure Disorders Fictitious Disorder or Malingering Age related memory changes
Depersonalization/Derealization Disorder A. The presence of persistent or recurrent experiences of depersonalization, derealization, or both B. During the depersonalization or dereaslization experiences, reality testing remains intact C. The symptoms cause distress or impairment D. The disturbance is not a function a substance or medication E. Not better explained by another disorder (e.g. PTSD, OCD, MDD, another Dissociative Disorder)
Depersonalization/Derealization Disorder Prevalence: About 50% of US adults will report at least one episode of Depersonalization or Derealization every year. However, to meet full criteria for this disorder is less common Life-Time Prevalence: 2.0% (gender ration 1:1) Developmental Course: Mean age of onset is 16-years (only 5% report onset after age 25, onset after age 40 is extremely rare) 1/3 experience a discrete episode, 1/3 report continuous SXS, and 1/3 report intermittent episodes that eventually become continuous
Depersonalization/Derealization Disorder Differential Diagnosis: MDD OCD Illness anxiety disorder Other Dissociative Disorders Anxiety disorders Psychotic disorders Substance/medication-related disorders Comorbidity: High with MDD and any anxiety disorder (except PTSD). Also often comorbid with Avoidant, Borderline, and Obsessive-Compulsive Personality Disorders
Treatments Psychotherapy is the First Line treatment (e.g. CBT, EMDR, DBT). Counseling is often trauma focused Focus: Improvement of coping skills Common Elements: Crisis response planning, removal from environment (if needed), labeling emotions, identifying triggers, building distress tolerance, coping skills training Some traditional DID Psychotherapies that involve discovery of alters have been shown to be harmful. Medications: Common medications include antidepressants, anxiolytics, and some atypical antipsychotics. Meds are considered secondary or adjunctive
References American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition/ Arlington, VA, American Psychiatric Association, 2013. International Society for the Study of Trauma and Dissociation, Dissociation FAQs (www.isst-d.org, 11/23/2016) Lilienfeld, S. (2007). Psychological Treatments that Cause Harm. Perspectives on Psychological Science 2 (1), 53-70.
 undefined
undefined