Digital Inclusion to Prevent Drug-Related Deaths: Literature Review Interim Report
This literature review explores how digital technologies can support individuals who use drugs and their families. It analyzes the effectiveness of various digital interventions in reducing harm, encompassing telehealth, mHealth, eHealth, and wearable technologies. The study identifies key areas for digital inclusion and highlights the impact of the COVID-19 pandemic on the adoption of digital solutions in this domain.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Digital Inclusion Digital Inclusion to Prevent Drug to Prevent Drug- - Related Deaths: Related Deaths: Literature review Literature review Interim Report May 2022
Dr Hadi Daneshvar, Dr Hannah Carver, Professor Catriona Matheson, Professor Tessa Parkes, Mr Joe Schofield and Mr Graeme Strachan. Authors Authors
How digital technologies have been used to support people who use drugs or their families and carers? How can digital technology support people who use drugs? Where and when are these services available? The aim of the The aim of the review review What technology will work for whom and in what circumstances/settings/stages of treatment/recovery? What evidence (qualitative and quantitative) supports the application of digital technologies to reduce harm to people who use drugs?
Rapid review using a systematic search strategy PRISMA flowchart shows the progress of search and selection papers Searched five academic electronic databases for articles published between January 2010 and August 2021 A comprehensive search of databases - related to drugs and digital inclusion/exclusion yielded 3,206 articles (after removing duplicates) Included papers peer-reviewed studies published in English in international journals, including all literature (qualitative and quantitative) comprising of review papers (systematic/narrative etc.) and empirical studies (including published conference papers) Excluded papers - protocols, conference abstracts, clinical trial registry, in-progress studies, frameworks with no empirical data, opinion-based articles or commentaries and non-digital intervention How did we go How did we go about this? about this? PRISMA flowchart for academic papers
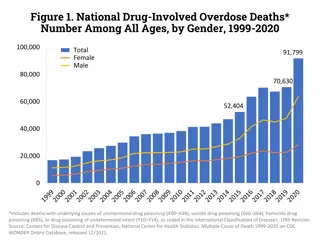
68 papers were identified and examined: 24 papers on Telehealth (the telephone and video intervention) 16 papers on mHealth (mobile health) 15 papers on eHealth (electronic health) 4 papers on sensors and wearable technologies Categories Matheson et al. (2022)* recommended nine topics as areas for Digital Lifeline Scotland. 38 of 68 papers were categorised into these nine topics. 30 papers which did not fall into these nine categories were labelled as other . This included telemedicine, examination of telehealth methods (e.g. text message, telephone-based) or analysis of m-health usage of drugs and telehealth management programmes. Overview of Overview of academic academic papers papers Pandemic Of the 68 papers, 75% (51 papers) were published after 2019 The COVID-19 pandemic has had a significant impact on the publication of papers in this field Pandemic has accelerated the implementation and use of digital technologies as a result of services having to move online or use digital technology In this slide deck, we present 7 categories of findings (out of a total of 9) which include a review of 22 papers with original data excluding reviews. * Matheson, C., Carver, H., Parkes, T., Daneshvar, H., Schofield, J., Dumbrell, J., Connell, C., Price, T. & Hnizdilova, K., 2022, Digital Inclusion to Prevent Drug-Related Deaths: Scoping user needs, Report to Digital Lifelines Scotland
1. Access to smartphone and data packages: Provision of smartphones and data packages Summary of Summary of findings: findings: Categories of Categories of 2. Provision of other digital technology e.g. computers, laptops and tablets: Access to computers, laptops and tablets to complement phone use, and facilitate more complicated online tasks. This could be via household provision, service-based, or another hub such as a community group. 3. Provision of support and skills training: Device provision should be supported by appropriate and tailored skills training needs needs 4. Improved access to the public Internet: Services providing access to public/hubs/internet cafes to support people with skills development generally but also to support practical use e.g. completion of online forms for specific purposes 5. Innovative skills training: Innovative skills training involving or led by PWUD 6. Development of local software applications: Website or software applications on local service availability 7. Development of digital services: Online chat (webchat) opportunities/functions in services or community groups
Seven papers related to this topic published from 2013 to 2021. All studies were conducted in the United States. mHealth based approaches may help interventionists reach a high-risk subgroup of people who use drugs who are highly dependent on methamphetamine and may be hard to reach using traditional intervention approaches. [1] Technology adoption and internet use were described as rising in people with substance use disorders. [2] 1. 1. Access to Access to smartphone smartphone and data and data packages packages Potential barriers exist to the successful implementation of mHealth and internet-based interventions for people who used drugs, particularly those who are older and have lower levels of income and educational attainment. [2] Patients have access to smartphones, but they may not be able to use all available features, particularly those requiring downloads and data usage. Methods to overcome such barriers may include providing patients with phone credit for research and/or treatment purposes, reverse charge phone and text services and free Wi-Fi in treatment services to download and use apps.[3] Lack of knowledge was identified as the reason for non-internet use. [4] Mobile phones are feasible and desired to deliver treatments that provide support to caregivers of teens discharged from substance use disorder treatment. Consideration should be given to the age of caregivers when designing these programmes. [5] Access to mobile phones significantly increased over time. Mobile phone ownership ranged from 64% in a study from 2013 to 94% in a 2018 study. [6] Mobile phones represent a common and ubiquitous technology among substance use disorder treatment patients, but interventions should be sensitive to frequent phone number changes that tend to occur with pay-as-you-go contracts.[7]
Two studies, conducted in the UK in 2015 and Greece in 2021, covered this topic The majority of people who use drugs use some type of information and communication technology (ICT), with a preference for smartphones. [8] 2 2. . Provision of Provision of other digital other digital technology e.g., technology e.g., computers, computers, laptops and laptops and tablets tablets Age, from the personal characteristics of the people who use drugs, was an important factor in the use of smartphones and the internet. Young adults had a significantly higher rate of use of Internet-based technologies.[8] Not everyone in one study was positive about ICTs and a few were decidedly negative. [9] Ownership of ICT does not guarantee their use, since individuals must both want and know how to engage with that technology. [9] People who use drugs were keen to engage with technology precisely because this was a means of being like everyone else. Despite this, they often lacked knowledge of ICTs and were deterred from their use by concerns that they might overspend and get into debt. From this, it would seem that, in relation to ICTs, levels of cultural capital amongst participants were generally high whilst human capital (in the form of education, knowledge, and skills) was significantly lower.[9] People who use drugs who also experience homelessness who had physical access to phones and computers, often, could not take full advantage of them because they had nobody to explain what their devices could do or to show them how they worked (i.e. their social capital was low). [9]
Two US papers and one EU paper published from 2019 to 2021, mentioned this topic but only indirectly As mentioned in slide 3, patients have access to technology, but they may not be able to use all available features, particularly those requiring downloads and data usage.[3] It showed a need for support and training. Problems with lack of face to face contact: A large number of individuals struggled with having little physical contact during COVID-19, which extended to telecare for group meetings and treatment. Some participants mentioned that clients had told them that group meetings by video doesn t feel normal, and that it s missing that connection and comfort. [10] Some resisted telecare by refusing to use it. This included resistance to the use of devices and online applications. Some people developed complex strategies to avoid being monitored by healthcare workers or authorities.[10] Knowledge and utilisation of technology-based interventions among health workers in the drug addiction field is low. Nevertheless, technology-based interventions are perceived as a possible means of facilitation in providing access to treatment. The need to improve training policies, awareness and attitudes towards technology-based interventions among EU health professionals, working in the field of addiction was considered paramount. [11] No study was identified evaluating training directly. However, as the findings above conclude, training and offering support to enhance digital skill are needed. 3 3. Provision of . Provision of support and support and skills training skills training
Two papers from India and the United States from 2021 related to this topic Participants use of mobile phones in India and their interest in mHealth interventions were assessed, most were not aware of the online availability of information related to substance use or its associated diseases. [12] Most participants reported accessing the internet through their mobile phones rather than relying on desktops or laptops.[12] The proportion of individuals having Internet access was much higher in this study than that reported in the survey of the general population in India.[12] As the majority of participants have used text message, authors suggested the simplest mHealth intervention could include sending text messages.[12] Other complex mHealth interventions such as creating mobile apps were suggested by authors, as > 60% of participants reported that they could download and use mobile apps. [12] In the US study providers noticed that patients were missing fewer appointments because of the convenience of telehealth. [13] Counselling via telehealth gave an opportunity to observe the patient s home environment and to engage family members.[13] Medication management via telehealth was considered less effective than in-person medication management.[13] 4 4. . Improved Improved access to the access to the public Internet public Internet
Three US papers related to this topic published from 2019 to 2021 Different innovation skills were introduced across three studies. [14, 15, 16] 1 A pilot of a telehealth programme to bring reproductive health care to women with opioid use disorder in a rural area was described. [14] 2 An evaluation of a six-month pilot programme which paired the services of a family planning clinic with community organisations to provide educational sessions was undertaken. [15] 5 5. Innovative . Innovative skills training skills training Findings recommended to service providers for women who use drugs, that innovative health care models such as the on-site provision of reproductive health care through telehealth have the potential to increase access to reproductive care for this hard-to-reach population. [15] 3 A pharmacist led telehealth clinic for overdose prevention highlighted: [16] People who use drugs showed a trend toward lower rates of prescribing through the clinical video telehealth clinic compared to all other clinics [16] Telehealth could be used for promoting the use of and education about naloxone [16]
Two US papers published from 2019 to 2021 described software applications The first paper considered telemedicine and remote treatment solutions specifically o Provision of video counselling software for virtual group meetings o The residential facilities provided the technology resources to staff working remotely to conduct individual and group therapies, case management, and recovery support. [17] 6 6. . Development Development of local software of local software applications applications The high use of technology and digital platforms, along with the differences in the type and preference of specific platforms and activities, underscored the importance in conducting formative research by programme developers, to determine the preferred location at which the targeted population would like to receive interventions.[18] Development of digital interventions should be informed by trends in user features .[18] Differential use of user features will allow for an informed design and dissemination of intervention programs that are more likely to be adopted by the target audience. For example, if the target audience is adolescents, the data suggest that a texting platform solution would be preferred. Similarly, results suggest that using instant messaging functions may be more impactful for targeting adolescents, while it may be less beneficial for targeting young adults. Further, the younger generation may respond to recovery messages formatted in the way of news as well as exaggerated messages with cartoons that use humour to teach important skills. [18]
Four US papers related to this topic, largely related to the pandemic, were published from 2020 to 2021 Two papers assessed the pandemic s impact on services and how it affects the services from different angles [19 & 20]. 7 7. . Before the pandemic the centres that provide treatment for opioid use disorder did not show any interest in the adoption or use of telehealth services [21] but the pandemic pushed them to move forward toward this approach. Development Development of digital of digital services services The pandemic prompted adaptation to some peer recovery specialists roles and responsibilities as those services moved online. [19] The virtual option to join meetings and engage in telehealth decreased barriers to treatment for some clients, such as transportation or extra time to commute. [19] Technological challenges and resistance to the use of technology such as client lack of access to technology, and lack of knowledge, lead to limited use of technology [19]. During the pandemic, policymakers changed or relaxed regulations that hindered access to treatment for people who use drugs. The majority of telehealth facilities were accepting new patients. [20] Given that future pandemics or disasters may also require a rapid pivot to telehealth, more research and planning are needed to understand how best to initiate new patients into substance use disorder treatment via telehealth. [22]
The pandemic has provided a rapid escalation in digital support for people who use drugs. Although there was a large volume of literature, mostly from the US, none was specific to reducing the risk of overdose and drug-related death. Summary Summary The lack of UK literature highlight the importance and novelty of the provision of digital connection and solutions through the Digital Lifelines Scotland programme.
References: 1. Collins, K. M., Armenta, R. F., Cuevas-mota, J., Liu, L., Strathdee, S. A. & Garfein, R. S. 2016. Factors associated with patterns of mobile technology use among persons who inject drugs. Substance Abuse. 2. Genz, A., Kirk, G., Piggott, D., Mehta, S. H., Linas, B. S. & Westergaard, R. P. 2015. Uptake and Acceptability of Information and Communication Technology in a Community-Based Cohort of People Who Inject Drugs: Implications for Mobile Health Interventions. Journal Medical Internet Research: mHealth uHealth. 3. Milward, J., Day, E., Wadsworth, E., Strang, J. & Lynskey, M. 2015. Mobile phone ownership, usage and readiness to use by patients in drug treatment. Drug Alcohol Depend. 4. Ozga, J. E., Paquette, C., Syvertsen, J. L. & Pollini, R. A. 2021. Mobile phone and internet use among people who inject drugs: Implications for mobile health interventions. Substance Abuse. 5. Ryan-pettes, S. R., Lange, L. L. & Magnuson, K. I. 2019. Mobile Phone Access and Preference for Technology-Assisted Aftercare Among Low-Income Caregivers of Teens Enrolled in Outpatient Substance Use Treatment: Questionnaire Study. JMIR mHealth and uHealth. Summing up Summing up Key findings Key findings and Alcohol Dependence. 6. Ashford, R. D., Lynch, K. & Curtis, B. 2018. Technology and Social Media Use Among Patients Enrolled in Outpatient Addiction Treatment Programs: Cross-Sectional Survey Study. Journal of Medical Internet Research. 7. Mcclure, E. A., Acquavita, S. P., Harding, E. & Stitzer, M. L. 2013. Utilization of communication technology by patients enrolled in substance abuse treatment. Drug 8. Mimigiannis, C., Gallos, P. & Mantas, J. 2020. The Drug Addicts' Usage of Information and Communication Technologies. Studies in Health Technology and Informatics. 9. Neale, J. & Stevenson, C. 2014. Homeless drug users and information technology: A qualitative study with potential implications for recovery from drug dependence. Substance Use and Misuse. 10.Caulfield, C. P. 2021. Using Telecare to Treat Opioid Use Disorder: An Ethnographic Study in New York During COVID-19. Contemporary Drug Problems. 11.Quaglio, G., Pirona, A., Esposito, G., Karapiperis, T., Brand, H., Dom, G., Bertinato, L., Montanari, L., Kiefer, F. & Carr , G. 2019. Knowledge and utilization of technology-based interventions for substance use disorders: An exploratory study among health professionals in the European Union. Drugs: Education, Prevention & Policy.
References: 12. Ganesh, R., Rao, R., Deb, K. S., Bhad, R. & Yadav, D. 2021. Digital Capacity and Interest in mHealth Interventions Among Individuals on Opioid Agonist Maintenance Treatment: A Cross-Sectional Community-Based Study. Indian Journal of Psychological Medicine. 13. Mark, T. L., Treiman, K., Padwa, H., Henretty, K., Tzeng, J. & Gilbert, M. 2021. Addiction Treatment and Telehealth: Review of Efficacy and Provider Insights During the COVID-19 Pandemic. Psychiatric Services (Washington, D.C.). 14. Cantor, J., Mcbain, R. K., Kofner, A., Hanson, R., Stein, B. D. & Yu, H. 2021. Telehealth Adoption by Mental Health and Substance Use Disorder Treatment Facilities in the COVID-19 Pandemic. Psychiatric services (Washington, D.C.) 15. Thompson, T. A., Ahrens, K. A. & Coplon, L. 2020. Virtually possible: using telehealth to bring reproductive health care to women with opioid use disorder in rural Maine. mHealth. 16. Jensen, A. N., Beam, C. M., Douglass, A. R., Brabson, J. E., Colvard, M. & Bean, J. 2019. Description of a pharmacist-led clinical video telehealth group clinic for opioid overdose prevention and naloxone education. The Mental Health Clinician. Summing up Summing up Key findings Key findings Interventions Between Generation Z and Millennials in the Treatment of Substance Use: Cross-Sectional Questionnaire Study. Journal Medical Internet Research. 17. Kedia, S. K., Schmidt, M., Dillon, P. J., Arshad, H. & Yu, X. 2021. Substance use treatment in Appalachian Tennessee amid COVID-19: Challenges and preparing for the future. Journal of Substance Abuse Treatment. 18. Curtis, B. L., Ashford, R. D., Magnuson, K. I. & Ryan-pettes, S. R. 2019. Comparison of Smartphone Ownership, Social Media Use, and Willingness to Use Digital 19. Anvari, M. S., Seitz-brown, C. J., Spencer, J., Mulheron, M., Abdelwahab, S., Borba, C. P. C., Magidson, J. F. & Felton, J. W. 2021. "How can I hug someone now [over the phone]?": Impacts of COVID-19 on peer recovery specialists and clients in substance use treatment. Journal of Substance Abuse Treatment. 20. Cantor, J. & Laurito, A. 2021. The new services that opioid treatment programs have adopted in response to COVID-19. Journal of Substance Abuse Treatment. 21. Uscher-pines, L., Raja, P., Mehrotra, A. & Huskamp, H. A. 2020. Health center implementation of telemedicine for opioid use disorders: A qualitative assessment of adopters and nonadopters. Journal of Substance Abuse Treatment. 22. Henretty, K., Padwa, H., Treiman, K., Gilbert, M. & Mark, T. L. 2021. Impact of the Coronavirus Pandemic on Substance Use Disorder Treatment: Findings from a Survey of Specialty Providers in California. Substance Abuse: Research and Treatment.