Death Certification: A Comprehensive Guide for Clinicians
This reference guide delves into the purpose and responsibilities associated with death certification, covering topics such as completing the death certificate, pronouncement of death, and the clinician's role. It emphasizes the importance of accurate documentation for national statistics, medical research, and public health initiatives. The guide also discusses the process involved in certifying death, including considerations for cases with external causes or requiring autopsy.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CERTIFICATION OF DEATH: A REFERENCE GUIDE Douglas-Jarrett Cole Turno, M.S., P.A-C
OVERVIEW Purpose of Death Certification The Clinician's Responsibility Completing the Death Certificate: Medico-Legal Review, Organ/Tissue Donation, Cause of Death, Autopsy Consent and Remaining Points
PURPOSE Public record for national and state mortality statistics Determine aims for medical research and guide budgetary funding for particular morbid/mortal medical conditions Set public health goals Measure health status of a population (local -> national)
A CLINICIANS RESPONSIBILITY Completion of the medical component of the certificate with signatures in a prompt manner assists in the closure of the deceased s personal affairs Provider must be familiar with state/local regulations of deaths that may have external causes or occurred without witness and may be reportable to medical examiners office May require supplemental information in cases where an autopsy discovers different cause of death from one reported Cause of death on a death certificate succinctly communicates the same essential information as a case report
PRONOUNCEMENT Pronouncement of death can be made when the patient experiences irreversible cessation of circulatory and respiratory function If patient remains on artificial means of life support, death is pronounced when patient elicits irreversible cessation of a involuntary, spontaneous brain function Brain death must be ascertained prior to cessation of means of artificial circulatory and respiratory support
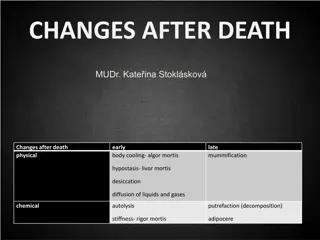
BRIEF PRONOUNCEMENT EXAM Testing Circulatory Respiratory Neurologic Exam Finding Pulseless for 2-5 min Apenic for 2-5 min Absence of cerebellar & brain stem function - Unresponsive to tactile or verbal stimuli for 2-5 min - Absent pupillary response - Absent ocular movements - Absent corneal reflex - Absent facial movement to noxious stimuli - Absent pharyngeal/tracheal reflex
COMPLETING THE CERTIFICATE 1. 2. 3. 4. 5. Use current, official form designated by the State in which death occurred Follow specified directions closely of each item on the form Use Black ink and make all entries legible Do NOT use any abbreviations be clear in your documentation Verify all personal information and spellings with deceased s designated informant , which is usually family Refer any issues not addressed on the form to the local registrar or State office of vital statistics Obtain ALL signatures from all involved providers; only use electronic authentication when permitted by the State Make no alterations and file the original document with the registrar timely, usually within 24 hours of event; complete form ideally within 60 minutes of patient s passing 6. 7. 8.
HIGHLIGHTING #7: PA S CAN SIGN THE REPORT OF DEATH Since July of 2016, in the Commonwealth of Massachusetts, a Physician Assistant is permitted to sign death certificates Chapter 133 48 of the Acts of 2016 amended M.G.L.c. 46 9 Ensure your institution has updated their bylaws to reflect current legislature
MEDICO-LEGAL STATUS Deciding to Report to Medical Examiner
REASONS TO CONTACT THE MEDICAL EXAMINER Non-medical Legal Death: death by natural causes Medical-Legal Death: any death where C.O.D is unknown, suspicious or unexpected and therefore requires further investigation Upon calling the Office of the Medical Examiner, the representative of that office will determine if the death of your patient warrants further inquiry after careful review of the case M.E. Office: 617-267-6767 *Provider must call the medical examiner s office to review the case and determine if the M.E. or coroner will assume jurisdiction of the case*
REASONS TO REFER TO MEDICAL EXAMINER Criminal violence Accidental or unintentional injury Trauma (i.e. non pathologic fracture) Skeletal remains Death related to dx/rx procedure Sudden death in person of otherwise good health Death within 24 hrs of admission (ACF or SNF) Death in public or private setting, prior to arrival to hospital Death of child < 2 years old or fetal death, >20 weeks gestation, wt > 350g Suicide Unusual or suspicious circumstance Occupational illness or injury
REASONS TO REFER TO MEDICAL EXAMINER Suspicion for abuse Prolonged loss of consciousness preceeding death (i.e. from time of admission to expiration) Death while in custody of law enforcement or mental health facility Death in emergency treatment facility, urgent care, walk-in or under foster care Toxidrome (drugs, alcohol, poison) Individual found dead Death of a pregnant woman during any stage of gestation, labor or delivery Death of a woman within 90 days of delivery or termination of pregnancy Any death occurring under such circumstances that the Office of the Medical Examiner deems appropriate
ORGAN/TISSUE DONATION In filing a report of death it is important to obtain consent from the patient s informant (whether that be family or a designated healthcare proxy or power or attorney) regarding organ donation All deceased individuals are potential donors
ORGAN/TISSUE DONATION If the patient or family declines donation, contact the New England Organ Bank (NEOB) and report the death as such. If the deceased IS an organ/tissue donor or family elects to donate patient s body, then proceed as noted below. Contact the New England Organ Bank at 24 hour number (1 800 446 6362) Discuss patient suitability for donation with NEOB Notate the name of the Donation Coordinator that you discussed the case with and indicate on the form whether or not patient is a viable candidate for organ/tissue donation
CAUSE OF DEATH A multi-part definition: A. Disease process or injury that directly led to events preceding death B. Circumstances in which death took place, whether violent, accidental or natural C. Entire sequence of events leading to death as well as medical conditions which significantly contributed to the death of an individual
CAUSE OF DEATH The cause of death section of the death certificate documentation dictates the medical opinion of the certifier on what led to the death of a patient It allows the certifier to document an etiological explanation of the order, type and association of events resulting in death. The initial condition that led to the death must be specific and must be accompanied by any injury, disease process, abnormality or poisoning that may have adversely affected the decedent
CAUSE OF DEATH The provider/certifier is responsible for documenting the chain of events leading to death Immediate cause of death (which ever final disease process, injury or complication resulting in death) must be written on line (A) Underlying causes (i.e. medical conditions, circumstances, injuries or complications) which directly led to death should be written on lowest lines (lines (B), (C), (D)) *Refer to Slide 25 for visual aid*
IMMEDIATE CAUSE OF DEATH Immediate COD: final disease process, injury or complication leading to death, generally to be listed on line (A) Do not list a mechanism of death or terminal event (i.e. cardiac or respiratory arrest) on line (A) as the mechanism is simply a statement that death occurred and does not explain the etiology of the event *Refer to Slide 25 for visual aid*
ANTECEDENT CAUSES OF DEATH To be listed on subsequent lines (B), (C) et cetera: but did not directly result in the death of the individual or were related to causes of death Any other important diseases or conditions that were present at the time of death the underlying One condition per line, listed chronologically from time of death Must document time approximate interval of cause to time of death (i.e. minutes, hours, months, years) Each subsequent line should provide an etiology to the line listed above *Refer to Slide 25 for visual aid*
C.O.D EXAMPLE A B C
DOUBT IN C.O.D If there is any doubt surrounding the cause of death, qualifying remarks should be denoted to reflect said uncertainties Enter Unknown when the certifier is unable to provide certain cause of death despite reasonable medical review and after all efforts have been exhausted to elucidate a cause of death an autopsy would be recommended in these situations
AUTOPSY CONSENT And Remaining Points
OTHER ITEMS Remaining aspects of the form are as follows: Autopsy status Manner of death/injury natural, suicide, homicide, accidental Female pregnancy status at time of death Tobacco use as contributor to death 1. 2. 3. 4.
AUTOPSY CRITERIA Unanticipated death Death during new therapeutic trial regimen Death within 48 hours of surgery or invasive diagnostic procedure Death on a psychiatric unit Intraoperative/Intraprocedural death Death incident to pregnancy or within 7 days of delivery C.O.D sufficiently obscured as would delay completion of death certificate Any death where there is opportunity of clarification of a disease process and/or teaching of house staff Death of infant/child with congenital malformation(s) Per request of family or legal guardian An autopsy consent form must be completed prior to conduction of an autopsy
AUTOPSY CONSENT There are two means of obtaining autopsy consent, pending the circumstances of a patient s death If circumstances surrounding the patient s death make the nature of the death of possible medical-legal significance, the Medical Examiner must be contacted, and if he/she accepts the death under their jurisdiction, the body will be placed in custody of the Office of the Medical Examiner for official autopsy by the forensic pathologist. Defer consent for autopsy if ME office accepts the case for review If circumstances are of non-medical-legal significance, and the Medical Examiner does not review the case, then permission for autopsy may be provided by the patient s closest living relative. A HEALTH CARE PROXY IS NOT AUTHORIZED TO GIVE CONSENT
AUTOPSY CONSENT MAY BE OBTAINED FROM FAMILY IN FOLLOWING ORDER: Deceased is a Married Individual Deceased is a Single Individual 1. 2. 3. 4. 5. Child of legal age Father or mother Brother or sister of legal age Grandparent Uncle, aunt or first cousin of legal age 1. Spouse, if surviving or not legally separated or divorced Child of legal age Father or mother Brother or sister of legal age Grandparent Uncle, aunt, first cousin of legal age 2. 3. 4. 5. 6. A person less closely related may not sign if there is a living person more closely related. Autopsy may be performed if the deceased signed consent prior to death
REFERENCES Sondik, E.J. et al (2003). Physicians handbook on medical certification of death.