Blood Anatomy and Functions
Explore the anatomy and components of blood, including its physical characteristics, functions such as transportation, regulation, and protection. Learn about blood components like plasma proteins, cellular elements, and their vital roles in maintaining homeostasis in the body.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
BLOOD AND ITS COMPONENTS
Fluids of the Body Cells of the body are serviced by 2 fluids blood composed of plasma and a variety of cells transports nutrients and wastes interstitial fluid bathes the cells of the body Nutrients and oxygen diffuse from the blood into the interstitial fluid & then into the cells Wastes move in the reverse direction Hematology is study of blood and blood disorders
Physical Characteristics of Blood Thicker (more viscous) than water and flows more slowly than water Temperature of 100.4 degrees F pH 7.4 (7.35-7.45) 8 % of total body weight Blood volume 5 to 6 liters in average male 4 to 5 liters in average female hormonal negative feedback systems maintain constant blood volume and osmotic pressure
Functions of Blood Transportation O2, CO2, metabolic wastes, nutrients, heat & hormones Regulation helps regulate pH through buffers helps regulate body temperature coolant properties of water vasodilatation of surface vessels dump heat helps regulate water content of cells by interactions with dissolved ions and proteins Protection from disease & loss of blood
Blood components 55% plasma: 7 to 8% dissolved substances (sugars, amino acids, lipids & vitamins), ions, dissolved gases, hormones most of the proteins are plasma proteins: provide a role in balancing osmotic pressure and water flow between the blood and extracellular fluid/tissues loss of plasma proteins from blood decreases osmotic pressure in blood and results in water flow out of blood into tissues swelling most common plasma proteins: albumin, globulins, clotting proteins (fibrin)
Blood: Cellular elements 45% of blood is the cellular elements or formed elements 99% of this (44.55% of total blood) is erythrocytes or RBCs formed by differentiation of hematopoietic stem cells (HSCs) in the red bone marrow of long bones and pelvis makes about 2 million per second! most numerous cell type in the body 4 to 6 million per ul blood as they mature in the marrow they lose most organelles and its nucleus lack mitochondria and cannot use the oxygen they transport for ATP synthesis lives only about 120 days destroyed by the liver and spleen liver degrades the hemoglobin to its globin component and the heme is degraded to a pigment called bilirubin - bile Iron(Fe+3) transported in blood attached to transferrin protein stored in liver, muscle or spleen attached to ferritin or hemosiderin protein in bone marrow being used for hemoglobin synthesis
1% found in the Buffy coat : -leukocytes (WBCs) and platelets (thromobocytes) -neutrophils: phagocytic properties -release lysozymes which destroy/digest bacteria -release defensin proteins that act like antibiotics & poke holes in destroying them -release strong oxidants (bleach-like, strong chemicals ) that destroy - releases cytokines that attract other neutrophils -eosinophils: parasitic defense cells -also involved in the allergic response -release histaminase slows down inflammation caused by basophils bacterial cell walls bacteria -basophils: heparin, histamine & serotonin -heighten the inflammatory response and account for reaction -monocytes: enter various tissues and differentiate into phagocytic macrophages -lymphocytes: T and B cells hypersensitivity (allergic)
Blood Plasma Composed of approximately 90 percent water Includes many dissolved substances Nutrients, Salts (metal ions) Respiratory gases Hormones Proteins, Waste products
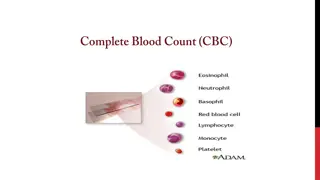
FORMED ELEMENTS OF BLOOD Red blood cells ( erythrocytes ) White blood cells ( leukocytes ) granular leukocytes neutrophils eosinophils basophils agranular leukocytes lymphocytes = T cells, B cells, and natural killer cells monocytes Platelets (special cell fragments)
Erythrocytes (Red Blood Cells) The main function is to carry oxygen Anatomy of circulating erythrocytes Biconcave disks Essentially bags of hemoglobin Anucleate (no nucleus) Contain very few organelles Outnumber white blood cells 1000:1
Contain oxygen-carrying protein hemoglobin that gives blood its red color 1/3 of cell s weight is hemoglobin Biconcave disk 8 microns in diameter increased surface area/volume ratio flexible shape for narrow passages no nucleus or other organelles no cell division or mitochondrial ATP formation Normal RBC count male 5.4 million/drop ---- female 4.8 million/drop new RBCs enter circulation at 2 million/second
Iron-containing protein Binds strongly, but reversibly, to oxygen Each hemoglobin molecule has four oxygen binding sites Each erythrocyte has 250 million hemoglobin molecules Globin protein consisting of 4 polypeptide chains One heme pigment attached to each polypeptide chain each heme contains an iron ion (Fe+2) that can combine reversibly with one oxygen molecule
Each hemoglobin molecule can carry 4 oxygen molecules from lungs to tissue cells Hemoglobin transports 23% of total CO2 waste from tissue cells to lungs for release combines with amino acids in globin portion of Hb Hemoglobin transports nitric oxide & super nitric oxide helping to regulate BP iron ions pick up nitric oxide (NO) & super nitric oxide (SNO)& transport it to & from the lungs NO causing vasoconstriction is released in the lungs SNO causing vasodilation is picked up in the lungs
Production of abnormal hemoglobin can result in serious blood disorders such as thalassemia and sickle cell anemia. The blood test, hemoglobin A1c, can be used to monitor blood glucose levels in diabetics
Hematocrit Percentage of blood occupied by cells female normal range 38 - 46% (average of 42%) male normal range 40 - 54% (average of 46%) testosterone Anemia not enough RBCs or not enough hemoglobin Polycythemia too many RBCs (over 65%) dehydration, tissue hypoxia, blood doping in athletes
Erythropoiesis: Production of RBCs Erythrocyte formation, called erythropoiesis, occurs in adult red bone marrow of certain bones. The main stimulus for erythropoiesis is hypoxia. Proerythroblast starts to produce hemoglobin Many steps later, nucleus is ejected & a reticulocyte is formed orange in color with traces of visible rough ER Reticulocytes escape from bone marrow into the blood In 1-2 days, they eject the remaining organelles to become a mature RBC
ANEMIA Symptoms oxygen-carrying capacity of blood is reduced fatigue, cold intolerance & paleness lack of O2 for ATP & heat production Types of anemia iron-deficiency = lack of absorption or loss of iron type of nutritional anemia failure to take in essential raw ingredients not made by the body pernicious = lack of intrinsic factor for vitamin B12 absorption from the digestive tract B12 is essential for normal RBC formation and maturation binding of B12 to intrinsic factor allows its absorption intrinsic factor synthesized by the small intestine
hemorrhagic = loss of RBCs due to bleeding (ulcer) hemolytic = defects in cell membranes cause rupture rupture of too many RBCs by external factors such as malaria (normal RBCs) or genetic disorders like sickle cell anemia (defective RBCs) thalassemia = hereditary deficiency of hemoglobin aplastic = destruction of bone marrow (radiation/toxins) failure of the bone marrow to produce enough RBCs may selectively destroy the ability to produce RBCs only but may also destroy the myeloid stem cells affect WBCs and platelets
WHITE BLOOD CELLS Leukocytes (white blood cells or WBCs) are nucleated cells and do not contain hemoglobin. Two principal types are granular (neutrophils, eosinophils, basophils) and agranular (lymphocytes and monocytes). Granular leukocytes include eosinophils, basophils, and neutrophils based on the straining of the granules. Agranular leukocytes do not have cytoplasmic granules and include the lymphocytes and monocytes, which differentiate into macrophages (fixed and wandering). Leukocytes have surface proteins, as do erythrocytes. They are called major histocompatibility antigens (MHC), are unique for each person (except for identical siblings), and can be used to identify a tissue.
Less numerous than RBCs 5000 to 10,000 cells per drop of blood 1 WBC for every 700 RBC Leukocytosis is a high white blood cell count microbes, strenuous exercise, anesthesia or surgery Leukopenia is low white blood cell count radiation, shock or chemotherapy Only 2% of total WBC population is in circulating blood at any given time rest is in lymphatic fluid, skin, lungs, lymph nodes & spleen
WBCs leave the blood stream by emigration. Some WBCs, particularly neutrophils and macrophages, are active in phagocytosis. The chemical attraction of WBCs to a disease or injury site is termed chemotaxis.
WBCs roll along endothelium, stick to it & squeeze between cells. adhesion molecules (selectins) help WBCs stick to endothelium displayed near site of injury molecules (integrins) found on neutrophils assist in movement through wall Neutrophils & macrophages phagocytize bacteria & debris chemotaxis of both kinins from injury site & toxins
Types of Leukocytes Granulocytes Granules in their cytoplasm can be stained Include neutrophils, eosinophils, and basophils Agranulocytes Lack visible cytoplasmic granules Include lymphocytes and monocytes
Granulocytes Neutrophils Multilobed nucleus with fine granules Act as phagocytes at active sites of infection Fastest response of all WBC to bacteria Direct actions against bacteria release lysozymes which destroy/digest bacteria release defensin proteins that act like antibiotics & poke holes in bacterial cell walls destroying them release strong oxidants (bleach-like, strong chemicals ) that destroy bacteria
Eosinophils Large brick-red cytoplasmic granules Found in repsonse to allergies and parasitic worms Leave capillaries to enter tissue fluid Release histaminase slows down inflammation caused by basophils Attack parasitic worms Phagocytize antibody-antigen complexes
Basophils Have histamine-containing granules Initiate inflammation Involved in inflammatory and allergy reactions Leave capillaries & enter connective tissue as mast cells Release heparin, histamine & serotonin heighten the inflammatory response and account for hypersensitivity (allergic) reaction
Agranulocytes Monocytes Largest of the white blood cells Function as macrophages Important in fighting chronic infection Take longer to get to site of infection, but arrive in larger numbers Become wandering macrophages, once they leave the capillaries Destroy microbes and clean up dead tissue following an infection
Lymphocytes Nucleus fills most of the cell Play an important role in the immune response B cells destroy bacteria and their toxins turn into plasma cells that produces antibodies T cells attack viruses, fungi, transplanted organs, cancer cells & some bacteria Natural killer cells attack many different microbes & some tumor cells destroy foreign invaders by direct attack
Platelets Derived from ruptured multinucleate cells (megakaryocytes) Needed for the clotting process Normal platelet count = 300,000/mm3
Thrombopoietin stimulates myeloid stem cells to produce platelets. Myeloid stem cells develop into megakaryocyte-colony- forming cells that develop into megakaryoblasts. Megakaryoblasts transform into megakaryocytes which fragment. Each fragment, enclosed by a piece of cell membrane, is a platelet (thrombocyte). Normal blood contains 250,000 to 400,000 platelets/mm3. Platelets have a life span of only 5 to 9 days; aged and dead platelets are removed by fixed macrophages in the spleen and liver.
Disc-shaped, 2 - 4 micron cell fragment with no nucleus Normal platelet count is 150,000- 400,000/drop of blood Other blood cell counts 5 million red & 5-10,000 white blood cells
HEMOSTASIS A clot is a gel consisting of a network of insoluble protein fibers (fibrin) in which formed elements of blood are trapped. The chemicals involved in clotting are known as coagulation (clotting) factors; most are in blood plasma, some are released by platelets, and one is released from damaged tissue cells. Blood clotting involves a cascade of reactions that may be divided into three stages: formation of prothrombinase (prothrombin activator), conversion of prothrombin into thrombin, and conversion of soluble fibrinogen into insoluble fibrin.
Stoppage of bleeding in a quick & localized fashion when blood vessels are damaged Prevents hemorrhage (loss of a large amount of blood) Methods utilized vascular spasm platelet plug formation blood clotting (coagulation = formation of fibrin threads)
Platelet Plug Formation Platelets store a lot of chemicals in granules needed for platelet plug formation alpha granules clotting factors platelet-derived growth factor cause proliferation of vascular endothelial cells, smooth muscle & fibroblasts to repair damaged vessels dense granules ADP, ATP, Ca+2, serotonin, fibrin-stabilizing factor, & enzymes that produce thromboxane A2 Steps in the process (1) platelet adhesion (2) platelet release reaction (3) platelet aggregation
Blood Clotting Blood drawn from the body thickens into a gel gel separates into liquid (serum) and a clot of insoluble fibers (fibrin) in which the cells are trapped If clotting occurs in an unbroken vessel is called a thrombosis Substances required for clotting are Ca+2, enzymes synthesized by liver cells and substances released by platelets or damaged tissues Clotting is a cascade of reactions in which each clotting factor activates the next in a fixed sequence resulting in the formation of fibrin threads prothrombinase & Ca+2 convert prothrombin into thrombin thrombin converts fibrinogen into fibrin threads
Prothrombinase is formed by either the intrinsic or extrinsic pathway Final common pathway produces fibrin threads
Extrinsic Pathway Damaged tissues leak tissue factor (thromboplastin) into bloodstream Prothrombinase forms in seconds In the presence of Ca+2, clotting factor X combines with V to form prothrombinase
Intrinsic Pathway Activation occurs endothelium is damaged & platelets come in contact with collagen of blood vessel wall platelets damaged & release phospholipids Requires several minutes for reaction to occur Substances involved: Ca+2 and clotting factors XII, X and V
Final Common Pathway Prothrombinase and Ca+2 catalyze the conversion of prothrombin to thrombin Thrombin in the presence of Ca+2 converts soluble fibrinogen to insoluble fibrin threads activates fibrin stabilizing factor XIII positive feedback effects of thrombin accelerates formation of prothrombinase activates platelets to release phospholipids
Anticoagulants and Thrombolytic Agents Anticoagulants suppress or prevent blood clotting heparin administered during hemodialysis and surgery warfarin (Coumadin) antagonist to vitamin K so blocks synthesis of clotting factors slower than heparin stored blood in blood banks treated with citrate phosphate dextrose (CPD) that removes Ca+2 Thrombolytic agents are injected to dissolve clots directly or indirectly activate plasminogen streptokinase or tissue plasminogen activator (t-PA)