Bacterial Pathogenesis: Key Concepts and Factors
Bacterial pathogenesis involves the ability of certain bacteria to cause disease by attributes such as transmissibility, adherence, motility, invasion, and toxigenicity. Pathogens can exploit host defenses, while virulence determines the severity of infection. Learn about opportunistic pathogens, non-pathogens, and the concept of infection, including the infectious dose required for different bacteria.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
BACTERIAL PATHOGENESIS Dr. Wasan Abdul-elah Bakir
Objective 1. Pathogenesis of bacterial infection 2. Stages of bacterial pathogenesis 3. Transmission 4. Bacterial virulence factors 5. Enzymes production 6. Pathogenicity islands 7. Typical stages if infectious disease
Pathogenesis of bacterial infection Most bacteria are harmless or often beneficial, some are pathogenic. For bacteria to cause disease (to be pathogenic) , it needs to have some attributes to help it reach the host and persist within the host and replicate, then causing harm (disease) to the host. Characteristics of bacteria that are pathogens are sometimes referred to as virulence factors : transmissibility adherence to host cells motility persistence invasion of host cells and tissues Toxigenicity the ability to evade or survive the host s immune system. Resistance to antimicrobials and disinfectants
The pathogen: A microorganism capable of causing disease in the host. Pathogenicity: is the ability of m.o to produce disease in a host. Opportunistic pathogens: are those that rarely, cause disease in immunocompetent people but can cause serious infection in immunocompromised patients. These opportunists are frequent members of the body s normal microbiota. Virulence: is the quantitative measure of pathogenicity, which is measured by the number of organisms required to cause disease. Virulent agents cause disease when introduced into the host in small numbers. Virulence involves adherence, persistence, invasion, and toxigenicity. Non pathogen: A microorganism that does not cause disease; may be part of the normal microbiota.
Infection: Multiplication of an infectious agent within the body. Multiplication of the bacteria that are part of the normal microbiota of the gastrointestinal tract, skin, and so on, is generally not considered an infection; on the other hand, multiplication of pathogenic bacteria (eg, Salmonella species) even if the person is asymptomatic is deemed an infection. The infectious dose: an organism required to cause disease varies among the pathogenic bacteria. For example, Shigella and Salmonella both cause diarrhea by infecting the gastrointestinal tract, but the infectious dose of Shigella is less than 100 organisms, whereas the infectious dose of Salmonella is on the order of 100,000 organisms.
The infectious dose of bacteria depends on their virulence factors (e.g., whether their pili allow them to adhere well to mucous membranes, or they produce exotoxins or endotoxins, whether they possess a capsule to protect them from phagocytosis, and whether they can survive various nonspecific host defenses such as acid in the stomach). Many, but not all, infections are communicable (i.e., they are spread from host to host). For example, tuberculosisis communicable (i.e., it is spread from person to person via airborne droplets produced by coughing), but botulism is not, because the exotoxin produced by the organism in the contaminated food affects only those eating that food. If a disease is highly communicable, the term contagiousis applied.
Many infections are asymptomatic or in apparent because our host defenses have eliminated the microorganism before it could multiply to sufficient numbers to cause the symptoms of disease. can be detected only by demonstrating a rise in antibody titer or by isolating the organism. Certain other infections lead to a carrier state: A person with asymptomatic infection that can be transmitted to another susceptible person.
Stages of bacterial pathogenesis Most bacterial infections are acquired from an external source. However, some bacterial infections are caused by members of the normal microbiota. A generalized sequence of the stages of infection is as follows: (1) Transmission from an external source into the portal of entry. (2) Evasion of primary host defenses such as skin or stomach acid. (3) Adherence to mucous membranes, usually by bacterial pili. (4) Colonization by growth of the bacteria at the site of adherence. (5) Disease symptoms caused by toxin production or invasion accompanied by inflammation. (6) Host immune response to each of the mentioned stages (7) Progression or resolving of disease.
The mode of transmission of many infectious diseases is human-to- human, but infectious diseases are also transmitted from nonhuman sources such as soil, water, and animals. Fomites are inanimate objects, such as towels, that serve as a source of microorganisms that can cause infectious diseases. Pathogens exit the infected patient most frequently from the respiratory and gastrointestinal tracts; hence transmission to the new host usually occurs via airborne respiratory droplets or fecal contamination of food and water. Organisms can also be transmitted by sexual contact, urine, skin contact, blood transfusions, contaminated needles, or biting insects.
Some bacteria that commonly cause disease in humans exist primarily in animals and incidentally infect humans. - For example, Salmonella and Campylobacter species typically infect animals and are transmitted in food products to humans. - The Clostridium species are ubiquitous in many environmental sources and are transmitted (eg, Clostridium perfringens gastroenteritis and Clostridium botulinum [botulism]) to humans by ingestion - or when wounds are contaminated by soil (eg, C. perfringens [gas gangrene] and C. tetani [tetanus])
modes of transmission of infection Pathogenic organisms can spread from one host to another by a variety of mechanisms. These include: Contact : a. Direct contact include sexually transmitted diseases such as syphilis, gonorrhea b. Indirect contact (via fomites such as clothes , pencils and drinking cups) Inhalation Droplet nuclei (such as meningococci and TB) Ingestion of food or drink contaminated by pathogens. Foodborne such as (dysentery) Waterborne such as (cholera ) Inoculation the pathogens can be inculcated directly into human skin or mucosa via different ways such as (wounds , burns ,doge bite, using contaminated needles and syringes). Insects
Congenital :Bacteria, viruses, and other microbes can also be transmitted from mother to offspring, a process called vertical transmission. The three modes by which organisms are transmitted vertically are 1. Across the placenta 2. Within the birth canal during birth 3. Via breast milk. Horizontal transmission isperson-to-person transmission that is not from mother to offspring. Iatrogenic and laboratory infections Pathogens transmission can happen for example during administration of injections, lumber puncture, exchange transfusion, dialysis, catheterization and other. Laboratory personnel handling infectious material.
Portals of entry The most frequent portals of entry of pathogenic bacteria into the body are the sites where mucous membranes meet with the skin, which are: The respiratory tract (upper and lower airways) Gastrointestinal (primarily mouth) Genital tract Urinary tract . Abnormal areas of mucous membranes and skin (eg, cuts, burns, and other injuries). - Normal skin and mucous membranes provide the primary defense against infection. -To cause disease, pathogens must overcome these barriers.
Many factors determine bacterial virulence or the ability to cause infection and disease. When bacteria enter the body of the host, and to cause infection, they must adhere to cells of a tissue surface. If they did not adhere, they would be swept away by mucus and other fluids that bathe the tissue surface. Adherence, which is only one step in the infectious process, is followed by development of colonies and subsequent steps in the pathogenesis of infection. Certain bacteria have specialized structures (e.g., pili) or produce substances (e.g., capsules or glycocalyces) that allow them to adhere to the surface of human cells, thereby enhancing their ability to cause disease. These adherence mechanisms are essential for organisms that attach to mucous membranes.
For example, the pili of Neisseria gonorrhoeae and E. coli mediate the attachment of the organisms to the urinary tract epithelium, and the glycocalyx of Staphylococcus epidermidis and certain viridans streptococci allows the organisms to adhere strongly to the endothelium of heart valves. After the bacteria attach, some bacteria form a protective matrix called a biofilm consisting of various polysaccharides proteins. Bacterial biofilms are aggregate or clusters of bacteria that are attached to a surface and/or to each other and embedded in a self- produced matrix.
Biofilms form on foreign bodies such as prosthetic joints, prosthetic heart valves, and intravenous catheters, but they also form on native structures such as heart valves. Biofilms may form on living or non-living surfaces and can be prevalent in natural, industrial and hospital settings. Help bacteria in a. persistence on surfaces, b. evasion of the immune response c. antimicrobial resistance d. dissemination. For example biofilms play an important role in the persistence of Pseudomonas in the lungs of cystic fibrosis patients.
2. Motility A huge advantage for bacteria to reach the host, and evade the immune system is for a bacterium to be motile to have the ability to direct its own movement. The bacterial flagellum is an amazingly complex machine with a diversity of roles in pathogenesis including reaching the optimal host site, colonization or invasion, maintenance at the infection site, and post-infection dispersal
After the colonization of bacteria, they multiply and then invade the body by spreading through tissues or via the lymphatic system to the bloodstream and cause bacteremia. This infection (bacteremia) can be transient or persistent. Bacteremia allows bacteria to spread widely in the body and permits them to reach tissues particularly suitable for their multiplication. Receptors for the bacteria on the surface of cells determine, the organs affected. For example, certain bacteria infect the brain because receptors for these microbes are located on the surface of brain neurons. Some bacteria (ex. Salmonella species) invade tissues through the junctions between epithelial cells.
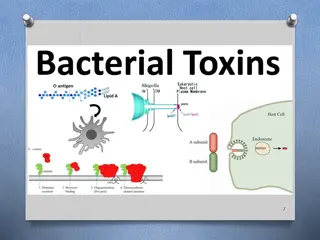
The major mechanism by which bacteria cause disease is the production of toxins. Toxins produced by bacteria are generally classified into two groups: A. Exotoxins B. Endotoxins
A- EXOTOXINS These toxins are produced by Many gram positive and gram negative bacteria. Exotoxins are antigenic and induce antibodies called antitoxins. When treated with formaldehyde or acid or heat, the exotoxin polypeptides are converted into toxoids, which are used in protective vaccines because they retain their antigenicity but have lost their toxicity. Toxoids, such as tetanus toxoid, are used to immunize against disease Exotoxins can be grouped into several categories (e.g., neurotoxins, cytotoxins, and enterotoxins) based on their biologic effect on host cells.
Many exotoxins have an AB subunit structure; the A (active or toxic) subunit possesses the toxic activity, and the B (binding) subunit is responsible for binding the exotoxin to specific receptors on the membrane of the human cell. Examples of exotoxines Neurotoxins: the toxins produced by Clostridium spp. for example, the botulinum toxin formed by C. botulinum. Cytotoxins: Corynebacteriumdiphtheriae. This cytotoxin inhibits protein synthesis in many cell types by catalyzing ADP-ribosylation of elongation factor II, which blocks elongation of the growing peptide chain. e.g. diphtheria toxin, which is produced by Enterotoxins: Exotoxins associated with diarrheal diseases are frequently called enterotoxins stimulate hypersecretion of water and electrolytes from the intestinal epithelium and thus produce watery diarrhea. e.g., shiga-like enterotoxin from E. coli, cholera toxin.
ENDOTOXIN (LIPOPOLYSACCHARIDES) The endotoxin {Lipopolysaccharide (LPS)} of gram-negative bacteria. It is a components of the cell wall of Gram-negative bacteria that are often liberated when the bacteria lyse. The substances are heat stable. They have three main regions: 1- The lipid A is the toxic component of LPS. It induces the overproduction of cytokines, such as TNF- and interleukin-1 from macrophages, which causes the symptoms of septic shock, such as fever and hypotension. (the lipid A moiety confers toxicity) 2- the core polysaccharide 3- an outermost O-antigen. Endotoxins are poorly antigenic, do not induce antitoxins, and do not form toxoids.
4. Enzyme production Pathogenic bacteria produce enzymes to degrade tissues infection. E.g Hyaluronidase and collagenase are hydrolyze hyaluronic acid and collagen respectively, constituents of the ground substance tissue. Immunoglobulin A (IgA) protease, which degrades IgA, allowing the organism to adhere membranes and spread enzymes that of connective to mucous Bacteria produce cytolysins which directly kill cells usually by forming pores in their membranes (e.g. hemolysins, leukocidins).
Large groups of genes that are associated with pathogenicity and are located on the bacterial chromosome are termed pathogenicity islands (PAIs). They are large organized groups of genes, usually 10 200 kb in size. Or The genes that encode many virulence factors in bacteria are clustered in pathogenicity islands on the bacterial chromosome. For example, in many bacteria, the genes encoding adhesions, invasions, and exotoxins are adjacent to each other on these islands.
The major properties of PAIs are as follows: They have one or more virulence genes They are present in the genome of pathogenic members of a species but absent in the nonpathogenic members They are large They typically have a different guanine plus cytosine (G + C) content than the rest of the bacterial genome They often have genetic instability Pathogenicity islands are found in many Gram-negative rods, such as E. coli, Salmonella, Shigella, Pseudomonas, and Vibrio cholerae, and in Gram-positive cocci, such as S. pneumoniae.
Antiphagocytic and other factors Capsule : The polysaccharide capsule prevents the phagocyte from adhering to bacteria. Encapsulated strains of many bacteria (such as Streptococcus pneumoniae and Neisseria meningitides ) are more virulent and more resistant to phagocytosis and non encapsulated strains. intracellular killing than Cell wall proteins of the gram-positive cocci, such as the M protein of the group A streptococci (Streptococci pyogenes) and protein A of Staphylococcus aureus. The M protein is antiphagocytic, and protein A binds to immunoglobulin G (IgG) and prevents the activation of complement
Intracellular survival Some bacteria survive intracellularly within the body cells such as macrophage and are shielded from humoral antibodies. These bacteria must possess specialized mechanisms to protect them from the harsh effects of the lysosomal enzymes encountered within the cell : 1. inhibition of the fusion of the phagosome with the lysosome, which allows the organisms to avoid the degradative enzymes in the lysosome. 2. inhibition of acidification of the phagosome, which reduces the activity of the lysosomal degradative enzymes. 3. escape from the phagosome into the cytoplasm, where there are no degradative enzymes.
A typical stages of acute infectious disease has four stages: (1) The incubation period, which is the time between the acquisition of the organism (or toxin) and the beginning of symptoms (this time varies from hours to days to weeks, depending on the organism). (2) The prodrome period, is the time during which nonspecific symptoms such as fever, malaise, and loss of appetite occur. (3) The specific-illness period, during which the overt characteristic signs and symptoms of the disease occur. (4) The recovery period, also known as the convalescence period, during which the illness abates and the patient returns to the healthy state.
DIFFERENT STRAINS OF THE SAME BACTERIA CAN PRODUCE DIFFERENT DISEASES Staphylococcus aureus causes inflammatory, pyogenic diseases such as endocarditis, osteomyelitis, and septic arthritis, as well as non pyogenic, exotoxine-mediated diseases such as toxic shock syndrome, scalded skin syndrome, and food poisoning. How do bacteria that belong to the same genus and species cause such widely divergent diseases? The answer is that individual bacteria produce different virulence factors that endow those bacteria with the capability to cause different diseases.
Further reading and material 1. Jawetz, Melnick, & Adelberg's Medical Microbiology; 28th edition; 2019 2. A Guide to Clinical Infectious Diseases, 16th edition 2020 Review of Medical Microbiology & Immunology: