Analysis of Pregnancy-Associated Deaths Due to Drug Overdose in Virginia (1999-2007)
This report examines pregnancy-associated deaths in Virginia from 1999 to 2007, specifically focusing on cases related to drug overdose. Among the 397 cases reviewed, substance abuse was found to be a significant contributor to 24.2% of deaths, impacting various causes and manners of death including accidents, homicides, and suicides. The data also shows the regional distribution of these cases and highlights the maternal mortality ratio associated with drug overdose. Insights into the health planning regions of residence for affected individuals are discussed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
VIRGINIA MATERNAL MORTALITY REVIEW TEAM Pregnancy-Associated Deaths Due to Drug Overdose in Virginia, 1999-2007 1
CASE DEFINITION: PREGNANCY- ASSOCIATED DEATH Death of a Virginia resident who was pregnant when she died or had a pregnancy in the year prior to death regardless of the cause of death or the outcome of the pregnancy. 2
Cause/Manner of Pregnancy-Associated Death in Virginia, 1999-2007, N=397 Number Motor Vehicle Accident Homicide Cardiac Disorder Cancer Accidental Overdose Suicide Percent 15.4 13.1 11.3 8.8 8.6 6.8 61 52 45 35 34 27 3
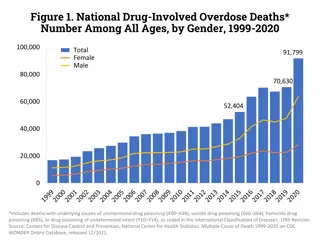
SCOPEOFTHESUBSTANCEABUSE PROBLEM Between 1999-2007, there were 397 cases of pregnancy-associated death in Virginia. Of all cases reviewed, 96 (24.2%) were determined to have substance abuse as a contributor to death. Substance abuse contributed to deaths resulting from violence as well as those due to natural causes. Among the causes and manners of death in which substance use contributed were motor vehicle accidents, infections, cardiac disorders and cardiomyopathies, homicide, and even suicides that were not caused by overdoses. 4
HEALTH PLANNING REGIONOF RESIDENCE FORTHE 94 CASESIN WHICH SUBSTANCE ABUSEWASA CONTRIBUTOR Substance Use Contributed to Pregnancy-Associated Death in Virginia by Health Planning Region of Residence, 1999-2007 (n=94) Number Percent Rate1 Northwest 8 8.5 6.3 Northern 16 17.0 5.6 Southwest 27 28.7 20.8 Central 28 29.8 19.0 Eastern 15 16.0 6.6 1The rate reflects the number of pregnancy-associated deaths for every 100,000 live births. 5
THE FOCUSOFOUR REPORT: DEATH WAS ATTRIBUTEDTO DRUG OVERDOSE 41 Cases (10.3% of all cases reviewed) Manner of Death: Accident (n=34), Suicide (n=6), Undetermined (n=1) Maternal Mortality Ratio = 4.5/100,000 live births 6
Health Planning Region of Decedents Residence, 1999-2007 (N=41) Number Percent Rate Northwest 3 7.3 2.3 Northern 6 14.6 2.1 Southwest 12 29.3 9.3 Central 11 26.8 7.5 Eastern 9 22.0 3.9 7
CHARACTERISTICSOF WOMEN DYING FROM DRUG OVERDOSES (N=41) Number Percent Race White Black Asian Other Age 19 and < 20-24 25-29 30-34 35-39 40-44 36 3 1 1 87.8 7.3 2.4 2.4 1 2.4 26.8 29.3 26.8 12.2 2.4 11 12 11 5 1 8
CHARACTERISTICSOF WOMEN DYING FROM DRUG OVERDOSES (N=41) Percent Number Marital Status Never Married Married Divorced Education < High School Completed High School More than High School Payment for Care No Care Self Pay Private Public Unknown 7 28 6 17.1 68.3 14.6 10 19 24.4 46.3 12 29.3 1 3 2.4 7.3 26.8 53.7 9.8 11 22 4 9
WHATARETHESOURCESOFTHE DRUGS? Causes of Death Number Percent Combined/mixed toxicity with at least one prescription One prescription drug 19 46.3 65.8 8 19.5 Over the counter/alcohol 3 7.3 Heroin 7 (+ ? 1 more) 17.1 (+2.4) 7.3 Stimulants 3 21 women (51.2%) had their own prescription for at least one substance. 10 women (24.4%) were poisoned by someone else s prescription medication. 10
A TYPICAL DECEDENT A typical decedent was a woman with a long, complex medical history with multiple physical complaints including chronic pain (migraines, back pain, abdominal pain) with numerous negative work-ups. She may also have had anxiety and/or depression. She was seen by multiple providers and called/visited their offices again and again for prescription refills. She frequently sought care in emergency departments too. 11
EXAMPLE Over 36 months, she filled 174 prescriptions for pain medications, antianxiety and antidepressants. Not included are prescriptions for other medical conditions. The prescriptions were written by numerous family practitioners, emergency room physicians and a few psychiatrists. Prescriptions were filled at various pharmacies within the same retail chain. Autopsy revealed no significant natural pathology. A high level of alcohol was found in the blood along with prescribed antidepressants. The levels of the prescription drugs were higher than normal ranges but far below fatal levels. Toxicity from them contributed to death but alcohol was the major drug responsible. 12
EXAMPLECONTINUED Toxicology found antidepressants at very high levels but not fatal in isolation. Benadryl was present in a high therapeutic level but not toxic. Hydrocodone was present in a therapeutic level and a benzodiazepine was present at a lower therapeutic level. All of these drugs contributed to death. Natural pathology did not contribute to death. 13
SYSTEMS FACTORS CONTRIBUTINGTO DEATHSDUETO OVERDOSE Lack of knowledge by emergency room and urgent care personnel in management of drug seeking patients and in dealing with mental health problems. Providers did not recognize the complex problems and difficult life circumstances of their patients. 14
SYSTEMS FACTORS CONTRIBUTINGTO DEATHSDUETO OVERDOSE Lack of multidisciplinary approach combining perinatal care, psychiatry, substance abuse treatment, and pain management. Inadequate support for providers in managing pregnant substance abusing women with chronic pain and/or drug seeking behaviors. 15
The Virginia Maternal Mortality Review Team urges a public health focus promoting the health of both mother and baby when developing policies to address these issues. 16
PROPOSED RECOMMENDATIONSFROMTHE MATERNAL MORTALITY REVIEW TEAM Recommendations for Resources and Guidance for Providers The American College of Obstetricians and Gynecologists (ACOG) should develop a Practice Bulletin on Pain Management in Pregnancy to serve as a resource for all providers of care to pregnant women. The Virginia Board of Health Professions and the Department of Behavioral Health and Developmental Services should develop a web- based resource guide utilizing evidence informed and promising practices for all licensed health care providers to assist them with referring substance misusing pregnant women to services. This document should be based on ASAM Placement Criteria for determining appropriate levels of treatment and should include a region by region description of available resources. 17
Recommendations for Provider and Public Education The Virginia Board of Pharmacy and the Virginia Department of Health should continue to develop tools to educate prescribers and dispensers on best practices for mitigating substance abuse and in routinely using the Prescription Monitoring Program to identify signs of potential abuse prior to issuing or dispensing a prescription. All professional organizations serving practitioners providing prenatal care such as the Virginia Section of ACOG; Virginia Affiliate of the American College of Nurse Midwives; Virginia Academy of Family Physicians; the Virginia Council of Nurse Practitioners; and the Virginia Chapter of the Association of Women s Health, Obstetric and Neonatal Nurses should encourage and train their membership to screen women throughout pregnancy for substance abuse, mental health problems, and intimate partner violence using a standardized screening protocol such as Screening, Brief Intervention, and Referral to Treatment (SBIRT) that is appropriate for pregnant women. 18
The Virginia Department of Health should work with home visiting programs to ensure they screen enrolled women throughout pregnancy for substance abuse, mental health problems, and intimate partner violence using a standardized screening protocol that is appropriate for pregnant women, for example, Screening, Brief Intervention, and Referral to Treatment (SBIRT), and connect them to appropriate services. The Virginia Section of ACOG; Virginia Chapter of the Association of Women s Health, Obstetric and Neonatal Nurses (AWHONN); and Virginia Affiliate of the American College of Nurse Midwives should hold a joint statewide summit biennially to educate providers on screening, referral and treatment of substance using women. 19
The Virginia College of Emergency Physicians and the Virginia Academy of Family Physicians should train Emergency Department staff and Urgent Care Center staff in use of the PMP; best practices for opioid prescribing; pain management; use of medically assisted treatment (MAT) in pregnancy; management of drug seeking patients; and in screening, identification, and referral of individuals at risk for substance abuse. The March of Dimes should expand their education campaign targeting the dangers of opioid misuse in pregnancy to include alcohol, tobacco, mood altering substances and other prescription medications. 20
Recommendations for Further Study The Virginia Section of the American College of Obstetricians and Gynecologists (ACOG) should provide a grant for a multicenter research project for OB/GYN residents to identify treatment needs and barriers among Virginia s pregnant women who misuse substances. The results should be widely distributed to the ACOG membership and participating institutions. The Handle with Care Workgroup being led by the Virginia Department of Behavioral Health and Developmental Services should assess the needs of medical providers throughout the state who provide care to pregnant women who use or may require a mood altering substance and develop a strategic plan to improve access to information, consultation and care coordination. 21
The Virginia Departments of Medical Assistance Services (DMAS) and the Department of Behavioral Health and Developmental Services (DBHDS) should develop a workgroup to identify barriers to increasing the number of enrolled Medicaid/FAMIS Methadone Clinics. DMAS, in working with its Behavioral Health Services Administrator (BHSA), and DBHDS should identify network recruitment strategies and potential clinics willing to participate in a pilot project to decrease network barriers. A proposed project goal is to decrease the administrative burdens on providers by streamlining billing for medically assisted treatment services for Medicaid and FAMIS MOMS eligible pregnant women who are opioid dependent. The Maternal Mortality Review Team supports the proposed recommendations of the Data/Monitoring Workgroup of the Governor s Prescription Drug and Heroin Abuse Task Force for action and/or study relating to providing additional clinical information in the Prescription Monitoring Program to prescribers and dispensers; improving logistics regarding use of Prescription Monitoring data which includes daily reporting of dispensed prescriptions; and reviewing how drug overdose, dispensing and PMP information is available to law enforcement/regulatory boards. 22
Contact Information Victoria Kavanaugh Maternal Mortality Review Team Coordinator Office of the Chief Medical Examiner 400 East Jackson Street Richmond, VA 23219 804.205-3853 Victoria.kavanaugh@vdh.virginia.gov 23