Achieving Comparable Results in Laboratory Practice
Good laboratory practice necessitates minimal error in measurement to reflect a patient's biological condition accurately, ensuring comparable and reliable results regardless of testing location or method. Standardization, harmonization, and traceability play crucial roles in achieving uniformity and accuracy in laboratory procedures, addressing calibration bias, imprecision, and sample influences. Comparable results are essential to prevent incorrect treatments and ensure consistent clinical guidelines, highlighting the importance of standardization and harmonization in the clinical laboratory. Methods such as using common traceable calibrators and monitoring performance through proficiency testing contribute to achieving comparable results in laboratory testing.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
STANDARDISATION, HARMONISATION AND TRACEABILITY Dr A A KHINE DIVISION OF CHEMICAL PATHOLOGY NHLS TYGERBERG STELLENBOSCH UNIVERSITY Laboratory Management workshop 3-6 June 2019
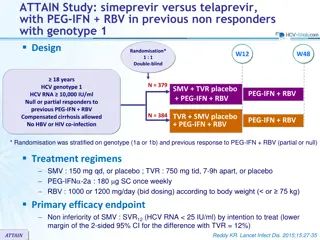
Good laboratory practice requires Error of measurement must be small enough that a result reflects a patient s biological condition. Comparable results that are independent of: Where and when a test was performed The measurement procedure used
Total Error Calibration bias to an accepted reference ( and also includes bias from calibrator lot-to-lot variability) Imprecision in a measurement procedure Sample specific influences non-specificity for the measurand interfering substances
Why We Need Comparable Results? If different measurements give different results for the same patient sample: Clinical practice guidelines become less useful. Patients may receive incorrect treatment. Patients may be moving around, thus specimens sent to various labs
Three areas of standardization in the clinical laboratory procedures that are followed before analysis How sample is analysed (test methods used) What calibrator is used and how it is traceable
Standardisation versus harmonisation Standardization: Same method or same instrument used Using calibrator with a traceability ref number Results are uniform among measurement procedures Reporting units are the same Harmonization: Different methods are used but results are not uniform but comparable Reporting units may not be the same originally but conversions help to make comparable (SI units) No reference measurement procedure and no pure substance reference material
How To Achieve Comparable Results? Laboratories using a common traceable calibrator or different calibrators with the same traceability ref number Performance is monitored and maintained by surveillance using proficiency testing (PT), external quality assessment (EQA), or a certification program.
Metrological traceability True value is not known unless it is attached to a reference so that value can be assigned is defined as the property of a measurement result whereby the result can be related to a reference through a documented unbroken chain of calibrations, each contributing to the measurement uncertainty . Traceability is established to SI using a reference calibrator and reference measurement procedure
COMMUTABILITY ISSUES Commutable means that the ref material reacts with the reagents in the ref method and other methods in the same way that analyte in the patient sample would Thus, values obtained from the calibration material and from native clinical samples have the same relationship across measurement procedures for the same measurand. Ideally a reference material should be validated for commutability against all field methods and types of samples but it is rarely the case Poor commutability means there is matrix effect affecting reaction between reagent and measurand
When there is no or poor commutability A manufacturer uses a master lot of calibrator that may be traceable to a non-commutable reference material, then the Traceability chain is broken Even though manufacturers claim traceability, the process fails to provide equivalent results for patient samples when different measurement procedures are used.
Calibration Traceability Does Not Ensure Accuracy for an Individual Patient Sample Measurement procedure may not be specific for the measurand. Measurand may not be well defined. Molecular form(s) of clinical interest Interfering substances present in a patient s sample may influence the result
Use of a Non-commutable Material for Calibration Will Cause Incorrect value assignment for the manufacturer s calibrator Incorrect results for patient samples
Calibrators in the routine laboratory A manufacturer's calibrator is proprietary (patented)- intended for use with a specific measurement procedure. It cannot be used with a different manufacturer s measurement procedure This is because the company has validated its commutability only with their own reagent
Change in Practice Needed In the business of producing and marketing PRM, SRM and TRM, there must be requirement to submit commutability validation against Reference methods Manufacturer s methods and reagents Routine clinical laboratory procedures and reagents A guideline for validating commutability is available: CLSI C53-A- Characterization and Qualification of Commutable Reference Materials for Laboratory Medicine (2010)
No traceability No reference measurement procedure or No reference material Can there be harmonisation?
Barriers to Harmonization Lack of a systematic process to identify and prioritize measurands Materials labelled as reference materials that have not been validated to be commutable for the intended measurement procedures Inadequate definition of the measurand Inadequate analytical specificity for the measurand Lack of systematic procedures to implement harmonization, in particular: When there is no reference measurement procedure When there is no reference material
Initiatives in establishing S and H IFCC has been a key leader in developing science in developing PRMs and RMPs. Many national and international groups are engaged JCTLM (joint committee for traceability in lab measurements) composed of three organizations: International Committee of Weights and Measures International Federation of Clinical Chemistry and Laboratory Medicine International Laboratory Accreditation Cooperation
Functions of JCTLM Maintain the list of reviewed and approved Reference measurement procedures Reference laboratories Reference materials Commutability requirements are being addressed.
Possibilities for consideration: Traceable to an all methods mean (outliers removed) of a panel of patient samples Traceable to a designated measurement procedure (arbitrary, but which has good correlation with clinical outcome)
References Mary Lou Gantzer, PhD, FACB. President, CLSI, CEO, BioCore Diagnostics. Laboratory Standardization: Bringing Order to Chaos Standardization the theory and practice-Jill Tate, M Panteghini The JCTML- A global approach to promote standardization of clinical laboratory test results Traceability, Reference systems and result comparability- Clin Biochem reviews- 28Aug 2007 ISO 17511
EXERCISE 1. What are the analytes in routine chemistry that have been standardized using both ref material and ref method procedure? 2. What are the analytes that have been standardized through development of primary ref material but not all routine laboratories use the reference method procedure? 3. What are the analytes that have been standardized through development of primary ref material but lacking method standardization? 4. What are the analytes that have not been standardized through both development of primary ref material or method standardization? 5. How has NHLS tried to harmonise the analytes under 2, 3, 4 and 5?