Addressing the Public Health Crisis: Innovative Strategies for Improved Health Outcomes
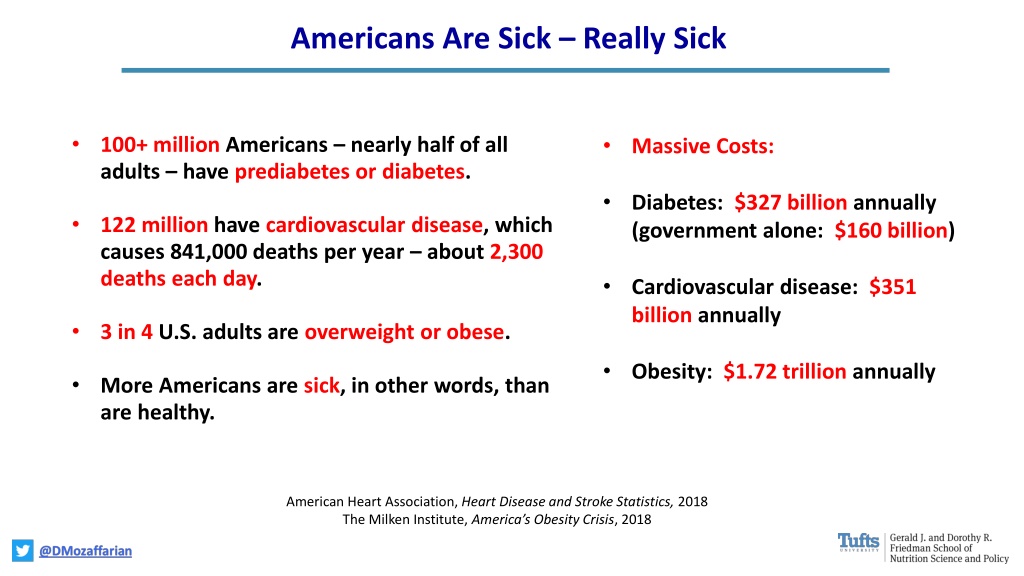
Over 100 million Americans suffer from conditions like prediabetes, diabetes, and cardiovascular diseases, resulting in staggering healthcare costs and mortality rates. This crisis calls for comprehensive approaches such as integrating food as medicine, promoting nutrition education, implementing healthy produce prescriptions, and providing medically tailored meals to improve health outcomes and reduce hospitalizations and costs.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Americans Are Sick Really Sick 100+ million Americans nearly half of all adults have prediabetes or diabetes. Massive Costs: Diabetes: $327 billion annually (government alone: $160 billion) 122 million have cardiovascular disease, which causes 841,000 deaths per year about 2,300 deaths each day. Cardiovascular disease: $351 billion annually 3 in 4 U.S. adults are overweight or obese. Obesity: $1.72 trillion annually More Americans are sick, in other words, than are healthy. American Heart Association, Heart Disease and Stroke Statistics, 2018 The Milken Institute, America s Obesity Crisis, 2018
Food is Medicine Nutrition Education for Providers: Medical licensing exams, specialty certifications, continuing medical education requirements Electronic Health Records: ACA standards, Fast Healthcare Interoperability Resources (FHIR) Produce Prescription Programs: Rx for free or discounted protective foods in healthcare settings, retail grocers, farmers markets, CSAs. Medically Tailored Meals: Coverage for home meals to high risk, food insecure patients with complex chronic conditions. Federal and State Cross-Agency Coordination: Synergies in aims and efforts, e.g. Medicare and senior nutrition programs; Medicaid and SNAP, WIC. Anchor Institutions Hospitals and Health Systems: Leverage ACA Community Health Needs Assessments and community benefit provisions for patient and community nutrition, e.g. summer meals, farmers' markets, senior nutrition programs, nutrition education. Value-Based Purchasing Models for Social Determinants: Address food insecurity and diet quality using Accountable Care Organizations, Accountable Health Communities, Medicaid Waivers.
Healthy Produce Prescriptions https://catalyst.nejm.org/prescribing-fresh-food-farmacy/ https://www.geisinger.org/freshfoodfarmacy
Medically Tailored Meals Providing home MTMs to chronically ill, food insecure patients dramatically reduces hospitalizations, ER visits, nursing home admissions, and costs. Using the 2011-2015 Massachusetts All Payers Database, MTMs: Reduce hospital admissions by 49% Reduce nursing facility admissions by 72% Save a net $9,036 per patient per year Number needed to treat (NNT): 2 per saved hospital admission, 1.1 per saved nursing facility admission http://www.fimcoalition.org/ Mozaffarian et al, JAMA Int Med 2019