Clinical Presentation and Management of a Possible Rabies Case in a 42-Year-Old Male
A 42-year-old male presented with back pain and an infected wound, later developing symptoms of fatigue, difficulty drinking water, muscle spasms, behavioral changes, and phobias. Concerns of possible Rabies led to admission, treatment with fluids, antivirals, and sedatives. Tetanus immunization was also administered, with further plans for diagnostic testing. The patient's non-cooperative behavior posed challenges in saliva collection for testing.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
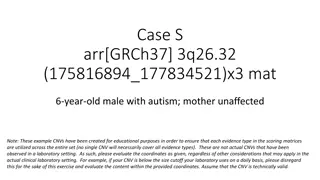
2023 ICD-10-CM Diagnosis Code A82.9 Javed Anees
Short Relevant History and Management in relation to Rabies Patients name :-Mr Binukumar,Age-42/Male This 42 year unmarried old manual labourer (tile work and painting job) chronic ethanolic ,smoker, stopped alcohol intake 2 days back presented with h/o low back pain, infected wound over his left upper leg with multiple excoriations over left lower thigh, attributed to injury with tiles.
2 days back he developed fatigue with intermittent shivering involving his limbs. He developed progressively increasing difficulty for drinking water, having severe pharyngeal muscle spasm on attempted drinking.
His behavioral change in the form of increased fearfulness,agitation,disoriented talk,spontaneous crying spells and emotional lability along with tremulousness of upper limb,trunk,limbs,and orthostatic tremor. He also has intolerance to wind (Aerophobic)
Examination Findings: Conscious,Orientation to Time and Place impaired and person partly normal. Other higher mental functions are within normal limits. Profuse sweating present,Emotional lability present, Aerophobia present, Hydrophobia present.Not allowing detailed examination. Plantar- B/l withdrawal,No neck stiffness Imp: Brainstem encephalitis- Probably viral
In view of significant hydrophobia with aerophobia, diagnosis of possible RABIES is made on clinical ground. And the patient was admitted in the isolation room, and started on -Full i/v fluids, Antiviral-(Ribavirin), Sedatives and muscle relaxants (Lorazepam and Baclofen)
In view of an infected wound along with muscle spasm, active tetanus immunization plus parenteral tetanus immunoglobulins were given. Plan: To sent samples of saliva and serum for PCR and Antibody test As patient was non cooperative,saliva collection was not possible
Adv: 1) Baseline imaging- NCCT/MRI Brain with Contrast 2) Continue inj.Ceftriaxone,Acyclovir,Antiepileptics 3) T.Lora 2mg 1-1-2 4) T.Quietiapine 25mg 0-0-1 5) CSF study- Virology studies (rabies virus study) 6) R/w with reports
Eosinophilic, sharply outlined, pathognomonic inclusion bodies (2 10 m in diameter) found in the cytoplasm of certain nerve cells containing the virus of rabies, especially in pyramidal cells within Ammon's horn of the hippocampus.
Definition:Rabies acute viral disease of the CNS affects all mammals transmitted by infected secretions, usually saliva. Bite of an infected animal (most common) Ingestion or transplantation of Contact exposures are through: with a virus-containing aerosol (occasional) infected tissues (may initiate the disease process)
Etiology Nucleocapsid antigen induces a complement-fixing antibody as well as T helper cell reactivity This is where antibodies to rabies virus (used in diagnostic immunofluorescence assays) are generally directed
Epidemiology Human infection occurs through: contact with unimmunized domestic animals exposure to wild animals in locales where rabies is enzootic or epizootic Common in : Southeast Asia;Philippines ;Africa ;Indian subcontinent ;Tropical South America
Corneal transplantation - several cases of human-to-human transmission of rabies have also been documented Bite and non-bite exposures to infected humans - could theoretically transmit rabies
ANIMAL SUSCEPTIBILITY TO RABIES: Very High: Foxes Coyotes Jackals Wolves Cotton rats High: Hamsters Skunks Raccoons Cats Bats Rabbits Cattle Moderate: Dogs Sheep Goats Horses Nonhuman primates Low: Opossum Rodents and lagomorphs - rarely infected with rabies virus.
Pathogenesis FIRST EVENT - Introduction of live virus through the epidermis or onto a mucous membrane INITIAL VIRAL REPLICATION- Within striated muscle cells at the site of inoculation Peripheral nervous system - Exposed at the neuromuscular and/or neurotendinous spindles of unmyelinated sensory nerve cell endings
Centripetal Spread : manner which the virus goes up the nerve to the CNS probably via peripheral nerve axoplasm, at a rate of ~3 mm/h replicates almost exclusively within the gray matter Centrifugal Spread : along autonomic nerves to other tissues: salivary glands, adrenal medulla, kidneys, lungs, liver, skeletal muscles, skin, and heart Passage of the virus into the salivary glands >viral replication in mucinogenic acinar cells> facilitate further transmission via infected saliva VIREMIA : Documented in experimental conditions no role in naturally acquired disease
Incubation Period : Exceedingly variable ranging from 7 days to >1 year (mean, 1 to 2 months) Apparently depending on the: Amount of virus introduced Amount of tissue involved Host defense mechanisms
Rates of infection and mortality as to site of inoculation are: Highest: from bites on the face Intermediate: from bites on the hands and arms Lowest: from bites on the legs Cases of human rabies with an extended incubation period (2 to 7 years) have been reported, but they are rare.
Clinical Manifestations: Four stages: 1. Nonspecific prodrome 2. Acute encephalitis similar to other viral encephalitides 3. Profound dysfunction of brainstem centers that produces the classic features of rabies encephalitis 4. Death or, in rare cases, recovery
1 Prodromal period Usually lasts 1 to 4 days and is marked by: fever headache malaise myalgias increased fatigability anorexia nausea and vomiting sore throat nonproductive cough Prodromal Symptom suggestive of rabies : at or around the site of inoculation of virus: Paresthesia and/or Fasciculations may be related to the multiplication of virus in the dorsal root ganglion of the sensory nerve supplying the area of the bite
2 Neurologic/Encephalitic Phase Encephalitic phase: Usually ushered in by periods of: excessive motor activity excitation agitation Clinical Features: Confusion Hallucinations Combativeness Bizarre aberrations of thought Muscle spasms Meningismus Opisthotonic posturing (the position of the body in which the head, neck, and spine are arched backwards)
2 Neurologic/Encephalitic Phase Periods of mental aberration Characteristically, are interspersed with completely lucid periods, but as the disease progresses the lucid periods get shorter until the patient lapses into coma Hyperesthesia, with excessive sensitivity to bright light, loud noise, touch, and even gentle breezes very common
Physical Examination: Temperature: may be found to be as high as 40.6 C (105 F). Abnormalities of the autonomic nervous system include: dilated irregular pupils increased lacrimation increased salivation, and increased perspiration postural hypotension. Upper motor neuron paralysis, with weakness, increased deep tendon reflexes, and extensor plantar responses
Paralysis of the vocal cords common Presenting signs and symptoms of rabies indistinguishable from those of other viral and neurologic diseases delays in diagnosis Hydrophobia or aerophobia : Seen in about two-thirds of recent cases presence increases the likelihood of antemortem diagnosis
3 Phase of Brainstem Dysfunction Manifestations begin shortly after the onset of the encephalitic phase Cranial nerve involvement causes: Diplopia Facial palsies Optic neuritis Difficulty with deglutition Difficulty in swallowing + Excessive salivation combination of produces the traditional picture of "foaming at the mouth." Hydrophobia : painful, violent, involuntary contraction of the diaphragmatic, accessory respiratory, pharyngeal, and laryngeal muscles initiated by swallowing liquids - seen in ~50% of cases
Amygdaloid nucleus involvement of the may result in: - priapism - spontaneous ejaculation Hypersexuality (has intense sex drives toward inappropriate animals or even inanimate objects, and loses all fear- and thus develops tameless as well) have been noted as a prominent feature in some
4 Death / Survival Patient lapses into coma + Involvement of the respiratory center Produces an apneic death Early brainstem dysfunction - Prominence distinguishes rabies from other viral encephalitides and accounts for the rapid downhill course
4 Survival Survival after the onset of symptoms - median period of 4 days - maximum of 20 days, unless artificial supportive measures are instituted Intensive respiratory support was mainstay in surviving Number of late complications may appear, includes: Inappropriate secretion of antidiuretic hormone diabetes insipidus cardiac arrhythmias vascular instability adult respiratory distress syndrome gastrointestinal bleeding Thrombocytopenia paralytic ileus RECOVERY very rare when it occurs, it is gradual
Varied Presentations: ASCENDING PARALYSIS: may also be a presentation of rabies resembling the Landry/Guillain-Barre syndrome (dumb rabies, rage tranquille) Initially, this clinical pattern was reported most frequently among persons given post-exposure rabies prophylaxis after being bitten by vampire bats. The difficulty of diagnosing rabies associated with this is illustrated by cases of person-to-person transmission of the virus by tissue transplantation
PARALYTIC RABIES : also occurs in Southeast Asia among persons with canine exposures CORNEAL TRANSPLANTS : if from donors who died of presumed Landry/Guillain-Barre syndrome produced clinical rabies in and caused the deaths of the recipients.
LABORATORY FINDINGS Hb values and routine blood chemistry : Early in the disease, are normal Abnormalities develop as hypothalamic dysfunction, gastrointestinal bleeding, and other complications ensue Peripheral white blood cell count : usually slightly elevated (12,000 to 17,000/uL) may be normal or as high as 30,000/uL.
The specific diagnosis of rabies: the isolation of virus from infected secretions [saliva or, rarely, cerebrospinal fluid (CSF)] or tissue (brain) the serologic demonstration of acute infection detection of viral antigen in infected tissue (e.g., corneal impression smears, skin biopsies, or brain), or detection of viral nucleic acid (RNA) by polymerase chain reaction (PCR). Reference laboratory evaluating antemortem samples can confirm rabies with high sensitivity and specificity
Most sensitive are: Isolation of virus from saliva Demonstration of viral nucleic acid in saliva, or Detection of viral antigen in a nuchal skin biopsy specimen Examination of corneal epithelium specimens appears less sensitive Demonstration of rabies antibodies in serum or CSF in the unvaccinated person, may be useful, although such antibodies may not appear until late in the course of disease
Samples of brain obtained at postmortem examination or brain biopsy should be subjected to mouse inoculation studies for virus isolation fluorescent antibody (FA) staining for viral antigen, and histologic and/or electron microscopic examination for Negri bodies or reverse transcription PCR for rabies virus RNA
Post exposure rabies prophylaxis rarely elicits CSF neutralizing antibody to rabies virus CSF neutralizing antibody to rabies virus If present after prophylaxis, it is usually found at a low titer (<1:64), whereas CSF titers in human rabies may vary from 1:200 to 1:160,000
Treatment National Guidelines for rabies prophylaxis-2019
Post-Exposure Prophylaxis The decision to initiate postexposure prophylaxis should include the following considerations: whether the individual came into physical contact with saliva or another substance likely to contain rabies virus whether rabies is known or suspected in the species and area associated with the exposure and the circumstances surrounding the exposure (e.g., whether the bite was provoked or unprovoked). Rabies is known or suspected to be present in the animal species animal should be captured if possible
The animal should be humanely killed: Any wild animal involved in a rabies exposure any ill, unvaccinated, or stray domestic animal involved in a rabies exposure Any animal inflicting an unprovoked bite, exhibiting abnormal behavior, or suspected of being rabid Animal's head should be sent immediately to an appropriate laboratory for rabies FA examination. Brain FA yields negative result it can be assumed that: the saliva contains no virus exposed person need not be treated
Persons exposed to wild animals that subsequently escape, that are capable of carrying rabies and that inhabit an area where rabies is known or suspected to be present - should undergo both passive and active immunization against rabies as soon as possible after exposure Area in which feline or canine rabies is not prevalent - Healthy biting dog, cat, or ferret can be confined and observed for 10 days - Persons should not begin a course of prophylaxis unless the animal develops clinical signs of rabies, animal becomes ill or behaves abnormally during the observation period
Animals that remain healthy for 10 days after a bite :- experimental and epidemiologic evidence suggests -will not have transmitted rabies Areas of high endemicity for canine rabies immediate examination of the animal's brain, especially in the case of a severe bite. Bites of rodents, rabbits, and hares - almost never require anti-rabies postexposure prophylaxis
Post exposure Prophylaxis Should be considered after direct contact between a human and a bat unless the exposed person can rule out a bite, scratch, or mucous membrane exposure Includes: rigorous cleansing treatment of the wound administration of rabies vaccine together with anti rabies immunoglobulin Should be initiated as soon as possible after exposure As the incubation period of rabies is quite variable, postexposure prophylaxis should be begun as long as clinical signs of rabies are not present
Wound cleansing and treatment: Thorough cleansing and treatment of the bite wound constitute an important component of rabies prevention The wound should be scrubbed with soap and then flushed with water. Both mechanical cleansing and chemical cleansing are important Quaternary ammonium compounds such as 1 to 4% benzalkonium chloride, 1% cetrimonium bromide, or povidone-iodine solutions
Passive immunisation PEP- administration of both passive antibody and vaccine, except when the individual has previously received preexposure prophylaxis Human rabies immune globulin (RIG) is preferred because equine antiserum may cause serum sickness RIG is administered only once, at the beginning of the postexposure prophylaxis regimen The recommended dose of RIG is 20 IU/kg The dose of equine antiserum is 40 units/kg. the full dose should be thoroughly infiltrated into the area around the wound and into the wound itself
Active Immunisation a. human diploid cell vaccine (HDCV), which can be given either intramuscularly or intradermally b. Rabies Vaccine Adsorbed (RVA) c. Purified Chick Embryo Cell Vaccine The latter two vaccines are administered intramuscularly Each vaccine is derived from a different strain of rabies virus and prepared in a slightly different formulation The three vaccines are considered equally efficacious and safe, and any of the three can be administered in conjunction with RIG
Pre Exposure Prophylaxis Given at individuals at high risk of contact with rabies virus, including: cave explorers veterinarians laboratory workers, and animal handlers Concomitant chloroquine administration interferes with the antibody response to rabies