Understanding Fungi: Characteristics and Types in Medical Mycology
Explore the world of fungi in medical mycology, including their characteristics, chemical tests, species differentiation, symptoms, diagnosis, and treatment. Learn about dermatophytosis, dermatomycosis, actinomyces, and the differences between fungi and bacteria. Discover the various types of fungi, such as molds, yeasts, and dimorphic fungi, with insights into their growth patterns.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Objectives By the end of this lecture the student must be: A) Identify the Characters of Fungi B) describe the chemical tests for this genus C) Differentiate between different sps. D) List and match the symptoms, diagnosis and treatment for different sps.
Medical Mycology Myco = Fungi Ology = Science Mycology is the science deals with fungi Mycoses = Fungal infection Dermatophytosis - "ringworm" disease of the nails, hair, and/or stratum corneum of the skin caused by fungi called dermatophytes Dermatomycosis - more general name for any skin disease caused by a fungus 2
What is the FUNGUS? Eukaryotic a true nucleus Do not contain chlorophyll Organoheterotrophic Cannot photosynthesize their own food Live either as saprophytes or parasites Have chitin cell walls Produce filamentous structures Reproduce by spores (sexual & asexual) Are aerobic life forms 3
What are Actinomyces? True Bacteria (Prokaryotic) Similar to fungi (fungi-like bacteria) WHY? 1. Clinical infection resembles mycoses 2. Grow on mycotic media 3. Grow slowly >48 h 4. Gross colonies resemble fungi (rough, heaped, short aerial filaments) 5. Resemble branched mycelia in tissue and smears mycelia microscopically, with 4
Fungi vs. Bacteria Bacteria Fungi Prokaryotes Eukaryotes Nucleus *Chitin Peptidoglycan Cell Wall Auto- or Heterotrophs Heterotrophs Nutrition Sexually & asexually Binary fission Reproduction E. coli Aspergillus Example Chitin is not found in any other microorganisms 5
Types of fungi 1. Multicellular: Molds- filamentous Penicillium, Aspergillus 2. Unicellular: Yeasts Candida, Cryptococcus 3. Dimorphic Fungi Dermatophytes, Histoplasma 6
YEAST Facultative Anaerobes Fermentation=ethanol and CO2 Non-filamentous unicellular fungi Spherical or oval Reproduction by Fission or budding 7
DIMORPHIC FUNGI Growth as a mold or as a yeast Most pathogenic fungi are dimorphic fungi At 37o C yeast-like At 25o C mold-like Can also occur with changes in CO2 Fungi grow differently in tissue vs nature/culture; often dictated by temp 8
Basic structure of fungi 1. Hyphae Main body of most fungi is made up of fine, Cylindrical, branching threads called hyphae Tubular cell wall filled with cytoplasm & organelles Most hyphae are 2-10 m diameter 2. Mycelia When formed of many cells, cellular units connect together (intertwining) to form long filamentous A. Aerial mycelium Part projects above the surface of medium B. Vegetative mycelium Part penetrate into medium and absorb food 9
Basic structure of fungi Septa regular cross-walls formed in hyphae Septate: Hyphae with septa - or Aseptate or coenocytic: Lacking septa except to delimit reproductive structures & aging hyphae Primary septa: Formed as a process of hyphal extension & generally have a septal pore, which allows for cytoplasmic & organelle movement Secondary or adventitious imperforate, formed to wall off ageing parts of the mycelium septa are 10
Reproduction Propagate via formation of spores Sexual and asexual spores The shape and type of spores are Different from one type of fungi to another Important in the classification & identification of different species of fungi 11
Asexual spore Conidiospore Multiple (chains) or single spores formed at the end of an aerial hypha Not enclosed by a SAC Aspergillus spp. Penicillium spp Conidiophore: filament that forms Conidospore 12
ConidioSpores Arthrospores Cells in hyphae develop thick wall & separate by disarticulation Coccidioides- genus of dimorphic Ascomycete Blastospores Thickened wall Bud from the parent cell Candida, Cryptococcus 13
Chlamydospores Spore contained within hypha Rounded & Thick cell wall Chlamydophores Aerial hypha with chlamydospores e.g. Candida albicans 14
Sporangiospore Spore contained in a sporangium at the end of a sporangoiphore Sporangium: A sac or cell containing spores produced asexually Sproangiophore- aerial hypha with sporangium Rhizopus spp 15
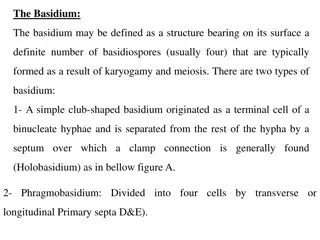
Sexual spores Sexual spores - exhibit fusion of nuclei Ascospore Formed in sac-like cell (ascus) Often 8 spores formed Ascomycetes Basidiospore Produced on a specialized club-shaped structure (basidium) Basidiomycetes Zygospore Thick-walled spore reproduction Zygomycetes/ Mucor and Rhizopus formed during sexual 16
Classification of Fungi Comprised of over 100,000 species Classified into 4 orders according to the presence or absence of sexual reproductive cycle and the nature of sexual spores Orders of Fungi 1. Zygomycetes 2. Ascomycetes Mycelium Non-septate Sexual Septate Reproduction Sexual 3. Basidomycetes Septate Sexual 4. Deutromycetes (Fungi imperfecti) Septate No sexual 17
ZYGOMYCETES Phylum Zygomycota/Sexual/Non-septate Lower fungi < 1000 species Produce zygospore, or sporangiospores Include the common bread molds and other fungi that cause food spoilage Mucor and Rhizopus are most familiar example 18
Ascomycetes Phylum Ascomycota, Septate/Sexual/Higher fungi Certain yeasts & some fungi that causes plant disease Contains more than 30,000 species of unicellular and multi-cellular fungi Produce sexual spores (ascospores) Produce asexual exospores (conidia) Unicellular e.g. Saccharomyces, Candida Multicellular e.g. Penicillum, Asperigullus, Claviceps, Dermatophytes, Sporothrix schenckii, Histoplasma 19
Basidomycetes Phylum Basidiomycota/Septate/Sexual Higher Fungi-Over 30,000 different species Sexual spores borne on clublike stalks (basidia) Mushrooms (Agaricus campestris) are the most familiar members Among Basidiomycota, & Cryptococcus are frequent human pathogens bisporus, Agaricus only Malassezia 20
Septate mycelium: Deutromycetes: Fungi imperfecti Sexual life cycle is either unknown or absent Reproduce by various types of asexual spores including budding Have an abundant mycelium at times while at other times they grow as yeast-like cells Includes majority of pathogenic to man & animal Resemble Ascomycetes in morphology Examples: Trichophyton, Microsporon, Candida, Cryptococcus, Histoplasma Epidermophyton, 21
Fungal cell wall composition Consists of 80% of polysaccharides Polysaccharide fibrils provide rigidity/integrity of wall 20% of the wall consists of Proteins 1. Structural components (Fibrous) A. Chitin microfibrils Polymers of (1-4)-linked N-acetylglucosamine B. Chitosan(in Zygomycota only) De-acetylated chitin C. -linked glucans Polymers of -1,3-linked glucose residues with short -1,6-linked side chains 22
Fungal cell wall composition 2. Matrix components (Gel-like components) Structural polymers are contained in gel-like matrix A. Mannoproteins Glycoproteins (form matrix throughout wall) B. (1,3) glucan 23
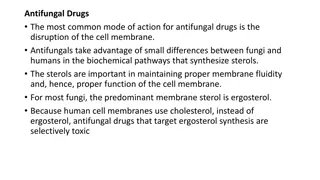
Structure of cell membrane Semi-permeable Phospholipid bilayer Involved in uptake of nutrients Anchorage for enzymes/proteins, e.g., chitin synthase, glucan synthase, etc. Signal transduction Differs in that it contains ERGOSTEROL Site of action for certain antifungal drugs Human cell doesn't contain ergosterol Human cell contains cholesterol 24
Medical Effect of Fungi I. Mycotoxicoses: Mould produces secondary metabolite (MYCOTOXINS) Highly toxic to humans Ingestion of toxic fungi or their metabolites Ergotism is caused by eating bread prepared from rye infected with Claviceps purpurea Historically, several large scale outbreaks of madness in populations have been attributed to ergotism Ergot are -adrenergic blockers inhibits response to adrenaline vasoconstriction necrosis gangaren Symptoms consisted of inflammation of infected tissue, followed by necrosis and gangrene 25
Medical Effect of Fungi Natural occurrence: Food products contaminated with AFLATOXINS include cereal (maize, rice & wheat), oilseeds (groundnut, soybean & cotton), spices (black pepper, coriander & zinger), tree nuts (almonds, and coconut) & milk Physical and chemical properties: Aflatoxins are potent toxic, carcinogenic, mutagenic, immunosuppressive agents, produced as secondary metabolites by Aspergillus flavus and A. parasiticus 26
Medical Effect of Fungi II. Hypersensitivity Disease: Fungal spores are inhalated They can be an antigenic elicit immune response production of Ig or sensitized lymphocyte Example is hypersensitivity pneumonitis 27
Medical Effect of Fungi III. Colonization and resultant disease: They may attack: 1. Outermost layers of Skin, hair and/or mucous membrane superficial mycoses 2. Epidermis as well as nail and hair cutaneous mycoses 3. Dermis, subcutaneous tissues, muscle and face Subcutaneous mycoses 4. The internal organs as the lungs, CNS, bones etc. systemic mycoses 5. Opportunistic - cause infection only in the immunocompromised 28
A. Superfacial mycosis 1. Tinea versicolor (Pityriasis versicolor) 2. Tinea nigra They are extremely superficial mycoses Primary Manifestation is pigment change of the skin Both are named for their respective skin manifestation 29
Tinea versicolor (Pityriasis versicolor) Causative agent: Malassezia globosa Less common-Malassezia furfur Lipophilic Yeasts belongs to Basidomycota Normal flora of skin and scalp Superficial opportunistic pathogens of the skin Associated with seborrheic dermatitis, dandruff (Pityriasis capitis) and atopic dermatitis Pityriasis versicolor is chronic superficial mycoses Characterized by a blotchy discoloration of skin which may itch With sunlight exposure the skin around patches will tan, but patches remains white 30
Pityriasis versicolor Chronic superficial mycoses Characterized by hyperpigmented lesions Well-demarcated white, pink, or brownish lesions, often coalescing and covered with thin furfuraceous scales The colour varies according to; The normal pigmentation of the patient exposure of the area to sunlight the severity of the disease. Lesions occur on the trunk, shoulders and arms, Rarely on the neck and face Fluoresce a pale greenish colour under Wood's ultra- violet light. 31
B. cutaneous Mycoses Dermatophytes attack keratinous structure of skin, hair and nail and cause the group of disease known as Ringworms or Tinea Candida can attack the skin, the mucous membranes and rarely the internal organs Non-dermatophyte moulds e.g. Hendrsonula toruloidea, Scytalidium hyalium, Scopulariopsis brevicaulis 32
i. Dermatophytes Confined to the outer layers of skin, hair & nails Do not invade living tissues Called dermatophytes (keratinophilic fungi) Produce extracellular keratinas hydrolyze keratin Utilize keratin for their nutrition Keratin is the chief protein in skin, hair and nail They caused dermatophycosis Ringworm" or Tinea" Dermatophycosis refers to the characteristic central clearing that often occurs in dermatophyte infections 33
I. dermatophytes 1. Trichophyton (19 species) Affect hair, skin & nails Infect both children & adults 2. Epidermophyton Infect skin, nails (rarely hair) Infect adults, rarely in children (ringworm) Epidermophyton floccosum 3. Microsporum (13 species) Affect hair, skin (rarely nails) Frequently in children, rarely in adults M. canis is the most common infect man 34
Ecology and Mode of transmission To determine the source of infection Anthrophilic Some Dermatophytes affect man only Person -to-person transmission through contaminated objects (comb, hat, etc.) T. rubrum and T. mentagrophytes Zoophilic Other affect animal mainly Direct transmission to humans by close contact with animals M. canis and T. verrucosum 35
Ecology and Mode of transmission Geophilic Other live in soil and can affect man Transmitted to humans by direct exposure M. gypseum Each geographic dermatophyton T. violaciumis the prevalent causative organism of Tinea capitis in Egypt M. audouiniis prevalent cause in England locality has its own 36
Tinea corporis Small lesions occurring anywhere on the body Causative agent: Trichophyton rubrum, T. mentagrophytes, M. canis, and M. audouinii Live on the skin surface (opportunistic) Reservoir: Humans, soil & animals Acquired by person-to-person transfer usually via direct skin contact with infected individual Animal-to-human transmission is common 37
Tinea pedis "athlete's foot" Infection of toe webs and soles of feet Causative agent: Trichophyton rubrum, Epidermophyton floccosum Requires warmth and moisture to survive and grow Causes scaling, flaking & itch of affected areas Reservoirs: Humans Athlete's foot is a communicable disease Transmission: when people who regularly wear shoes go barefoot in a moist environment T. mentagrophytes and 38
Tinea capitis Infection of the scalp Causative agent: Trichophyton and Microsporum invade the hair shaft Trichophyton infection prevail in Central America to USA & in parts of Western Europe Microsporum infection are in South America, Southern & Central Europe, Africa & Middle East Reservoirs: Humans & animals (dogs, cats and cattle) Transmitted by humans, animals or objects that harbor the fungus 39
Dermatophytes 4. Tinea cruris - "jock itch" Infection of the groin, perineum or perianal area Trichophyton rubrum Some other contributing fungi are Candida albicans, T. mentagrophytes and Epidermophyton floccosum. 5. Tinea barbae Ringworm of the bearded areas of the face and neck Trichophyton mentagrophytes and T. verrucosum 40
Dermatophytes 6. Tinea unguium (onychomycosis) Infection of nails Common - Trichophyton rubrum Less common- T. interdigitale, Epidermophyton floccosum, T. violaceum, Microsporum gypseum, T. tonsurans, T. soudanense Reservoirs: Humans and rarely animals or soil 41
Treatment of Dermatophytes All are sensitive to grisofulvin Tolfnatate available over the counter Topical Terbinifine (Lamisil) - oral, topical. Ketoconazole seems to be most effective for tinea versicolor and other dermatophytes Itraconazole - oral Echinocandins (caspofungin) 42
Lab diagnosis of Dermatophytes Specimen collection Skin Scrapings, nail scrapings and epilated hairs Direct Microscopy Specimens should be examined using 10% KOH and Parker ink or calcofluor white mounts Characteristic hyphae can be seen 43
Lab diagnosis of Dermatophytes Culture Specimens should be inoculated onto Sabouraud's dextrose agar (General purpose) Selective Mycosel agar Gentamicin: inhibits normal bacterial flora Cycloheximide: inhibits saprophytic fungi containing cycloheximide and incubated at 250C for 4 weeks The growth of any dermatophyte is significant 44
II. Candida Yeast-like organism that lives as a commensal in oral mucosa, throat, skin, scalp, vagina, fingers, nails, bronchi, lungs, or intestine and vagina Opportunistic organism The causative agent of candidiasis C. albicans, C. tropicalis & C. glabrata Candidiasis encompasses infections that range from superficial such as thrush and vaginitis Rarely become systemic in immunocompromised patients Septicaemia, endocarditis and meningitis 45
Symptoms of Candida albicans Thrush appears as creamy-white or bluish-white patches on the tongue - which is inflamed and sometimes-beefy red - and on the lining of the mouth, or in the throat. Diaper rash caused by candida is an inflammation of the skin, usually red and sometimes scaly. Vaginitisis characterized by a white or yellow discharge. Inflammation of the walls of vagina and of the vulva (external genital area) causes burning and itching. Infections of the fingernails and toenails appear as red, painful swelling around the nail. Later, pus may develop. 46
Laboratory diagnosis of candida Specimen: A scraping or swab of the affected area or blood (candidemia) is placed on a microscope slide Microscopic examination A drop of 10% KOH solution is added to the specimen. KOH dissolves the skin cells, but leaves Candida intact, permitting visualization budding yeast cells typical of many Candida species. Culture Swab/blood is streaked on a culture SDA medium The culture is incubated at 37 C for several days The characteristics of colonies may allow initial diagnosis of organism causing disease symptom of pseudohyphae and 47
Laboratory diagnosis of candida A germ tube test is a diagnostic test in which a sample of fungal spores are suspended in serum and examined by microscopy for the detection of any germ tubes It is particularly indicated for colonies of white or cream color on fungal culture, where a positive germ tube test is strongly indicative of Candida albicans 48
Treatment of candidacies Oral drugs: Amphotericin B, fluconazole, and ketoconazole, are the drugs most commonly used to treat candidiasis Topical administration of antifungal drugs such as clotrimazole, miconazole , tioconazole, and nystatin The drug of choice is nystatin 49
c. Subcutaneous Mycoses Rare Confined to subcutaneous tissue & rarely spread systemically Confined mainly to tropical regions Include heterogeneous group of soil fungal infections Introduced into the extremities by trauma/wound Tend to be slow in onset and chronic in duration The main subcutaneous fungal infections include Sporotrichosis, chromoblastomycosis, MYCETOMA, lobomycosis, rhinosporidiosis, zygomycosis, & subcutaneous phaeohyphomycosis50 subcutaneous