Tragic Tale of David James West: A Life Overshadowed by Mental Health Struggles
David James West, born prematurely with a traumatic birth, faced challenges from a young age due to intellectual giftedness and learning difficulties. He struggled with mental health issues, drug addiction, and ultimately succumbed to a drug overdose in 2013. Despite the family's efforts and interactions with mental health services, the system failed him, leading to a tragic end. The aftermath involved critical incident reports, complaints processes, and a struggle for justice and truth. This narrative sheds light on the complexities of mental health support and the devastating consequences when it falls short.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
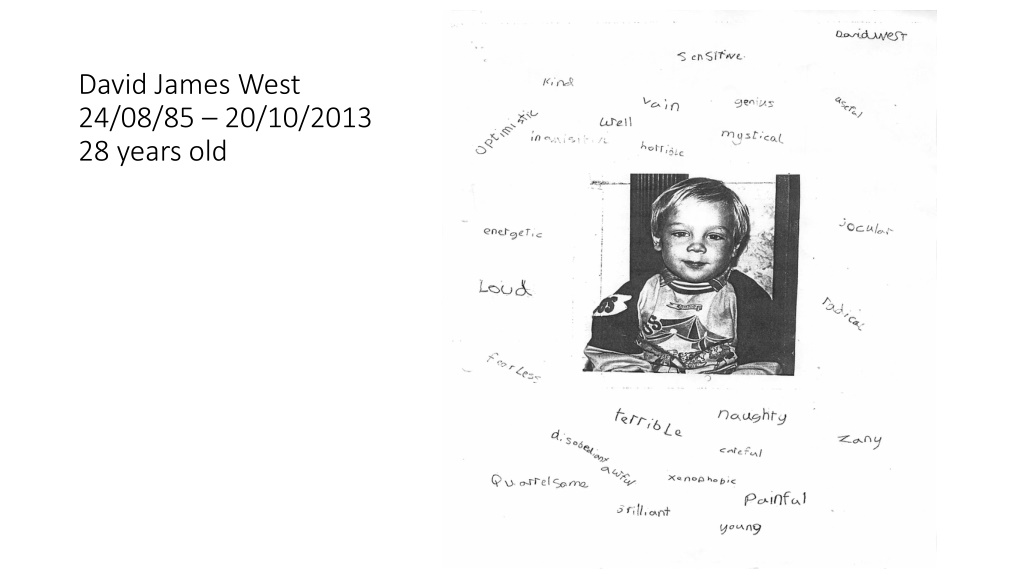
David James West 24/08/85 20/10/2013 28 years old
David James West born 24/08/1985. He was born 6 weeks premature, had foetal distress, traumatic birth, had forceps delivery and jaundice I believe he had a brain injury at birth. Eldest of 4 children. Very difficult early years IQ in top 1% of population intellectually gifted, member of MENSA Expelled from school aged 10. Special Educational Needs and difficulties. Left handed, had Dyspraxia, dyslexia and dysgraphia. Diagnosed with ADHD and given Ritalin. Was educated Monday to Friday at a special school and came home at weekends. Immature, lacking social skills and wanted instant results to his needs. Mismatch in his potential and what he achieved.
Drifted into drugs, became psychotic and had serious mental health problems sectioned under Mental Health Act many times. Diagnosis varied. Lots of anti psychotic medication given which did not help him but was like a cosh Came to Hampshire because of physical and financial abuse and was cared for by Southern Health NHS. Engaged and disengaged when it suited him moved around the area. Continued to take illegal drugs. His way of escaping from the world he lived in. Difficult life to lead self harmed and self neglected. He was a vulnerable person. My son died of an overdose of drugs in October 2013.
What happened Critical Incident Report completed by Southern Health Very concerned by contents of report The Doctor simply wrote on his patient notes Mental disorder due to multiple drug use. No underlying mental illness so he is responsible for the mental state he gets into when he takes drugs, just as substance abuser of Alcohol is. No role for AMH and he is toxic to such a service. Discharge from CCT. No letter. As a direct result of this Doctor s actions it meant my son was without medication, had no access to a GP or the Mental Health team for a period of about 10 weeks which left him in a dreadful mental state. Connor Sparrowhawk death Justice for LB - http://justiceforlb.org/ Later the Mazars report - https://www.england.nhs.uk/south/wp- content/uploads/sites/6/2015/12/mazars-rep.pdf 1000 deaths were not investigated.
The complaints process One year Independent investigation undertaken. Letter from Chief Executive of Trust Three days after letter from Chief Executive - Inquest: Coroner recorded death as being Death due to dependent misuse of drugs as a consequence of lifelong mental health problems. Reputational damage seemed more important to Southern Health than getting to the truth My background
Complaints process PHSO report We partly uphold Mr West s complaint. We have found failings in the care provided to David West. These include: failing to allocate a care coordinator failing to refer to Assertive Outreach or for a forensic assessment not updating Risk Assessments and Crisis, Relapse and Contingency Plans writing unprofessional and derogatory comments within medical records discharging from mental health services against the Trust s own policy on patients who do not engage or fail to attend appointments discharging from the Community Treatment Team and not communicating this decision not following relevant national NICE guidance failing to fully consider adult safeguarding policy failing to assess the need for aftercare under section 117 of the Mental Health Act 1983
Mental Health Code of Practice https://assets.publishing.service.gov.uk/government/uploads/system/upl oads/attachment_data/file/435512/MHA_Code_of_Practice.PDF The one thing that makes a difference is knowing that your voice is being heard and that we feel listened to by others Expert Ref Group service user
Not being listened to at Southern Health NHS Carolan report The strongest theme that emerged from the interviews with families, mentioned by almost all the families : Difficulty getting mental health workers to listen to them Not being able to access the level of support that was needed. A number of families suggested that the consequence of not being able to get appropriate, timely support was the death of their loved ones. Carolan Report Oct 2016 - Southern Health NHS file:///C:/Users/user1/Downloads/A%20review%20of%20family%20involvement%20in%20investigations%20conducted%20f ollowing%20a%20death%20at%20SHFT%20(2).pdf
GMC Complaint 5 year process GMC complaint One Doctor stuck off the medical register. GMC eventually admitted that the expert report that they used to initially determine that no action should be taken against a second Doctor was deficient and flawed. The complaint against the second Doctor resulted in admitted maladministration by the GMC and resulted in a Judicial Review and no action taken against the second Doctor.
Working with patients and families in investigations As soon as possible after a death speak to the family and have someone visit them that is trained in this important task. Ask if they have any concerns about the death. Explain what will happen Ask them how you can support them and do it. BE HONEST WITH THEM AND TELL THE TRUTH
What else happened at Southern Health - Inquest Ellie Brabant Inquest into death of Ellie Brabant 05/11 to 12/11/18 Self-inflicted death of Ellie Brabant - Coroner finding that the lack of a clear care plan, and the decision to discharge Ellie from Section 3 of the Mental Health Act more than minimally contributed to her death. Ellie, 28, was found hanging whilst an inpatient at Antelope House, a mental health unit in Southampton on 2 November 2017. She had spent most of her adult life detained under Section 3 of the Mental Health Act. Alice Stevens, Solicitor at Broudie Jackson Canter Solicitors, said: This is a deeply disturbing case. Ellie was a vulnerable patient with complex needs who was not afforded proper care and attention by those responsible for her care. The inquest was a frustrating process for Ellie s family with Trust staff disagreeing with independent experts who were highly critical of the care afforded to Ellie.
Inquest - Ellie Brabant In the months leading up to her death, Ellie was moved five times and spent time in a Psychiatric Intensive Care Unit due to escalating self-harm. Within nine days of residing in Antelope House, Ellie was made a voluntary inpatient. She subsequently utilised regular leave from hospital during which she reported being raped and taking drugs. A Prevention of Future Death report has been written by the coroner - Staff training around the importance of, and implementation, of observations of patients; Safeguarding of patients at risk of crimes and reporting these to police. The coroner noted that vulnerable patients like Ellie need to be safeguarded and further training on informal patients are needed; The coroner has also written to Southern Health Trust in relation to their conduct, including concerns about the preservation of evidence following serious incidents and late disclosure of evidence at the inquest.
Family and Inquest organisation view Ellie s family said: We are devastated by Ellie s death and the failures in her care at Antelope House. We were not given the opportunity to feed into Ellie s care and were instead left to watch her rapid decline. The Ellie who took her own life was not the Ellie we knew. Although we accept procedural changes have been made following Ellie s death, we do not believe these changes address the fundamental deficiency in Ellie s care. We do not feel confident that should another patient like Ellie be under Southern Health s care, anything would be done differently. Inquest Organisation said Once again, the conduct of Southern Health Trust suggests a greater concern about reputational management, rather than the opportunity to identify where they have failed to keep people safe. https://www.inquest.org.uk/inquest-concludes-ellie-brabant
Southern Health Now Fined over 2 million pounds for HSE offences where patients have died. Broken Trust TV programme - Whole Board changed - Execs and Non Execs. Three relatives have presented to the main Board about a compelling need to change and asked for 17 recommendations to be instigated in 2018. One of the most important will be the appointment of an IME. NHSI Appointed Nigel Pascoe QC - review the investigations of 5 deaths of patients. Pascoe report Published Feb 2020 https://www.england.nhs.uk/south- east/wp-content/uploads/sites/45/2020/02/060220-Report-pdf2.pdf Pascoe 2 - Public Investigation Hearings taken place April 2021 families declined to be involved. Report published Sept 2021. https://www.england.nhs.uk/south-east/publications/ind-invest- reports/southern-health/
Was his treatment by the NHS what he needed I believe that my son had a brain injury at birth He never had any test, brain scans or investigation. Given Ritalin at 9 years of age for ADHD.
Charles Dickens Tale of Two NHS Cities It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness, it was the epoch of belief, it was the epoch of incredulity, it was the season of Light, it was the season of Darkness, it was the spring of hope, it was the winter of despair, we had everything before us, we had nothing before us, we were all going direct to heaven, we were all going direct the other way
NHS Behcets Clinic London 1995 2012 - Doctor s treating me - GP who knew nothing about Behcet s disease and a Rheumatologist in London who was a specialist in Behcets. 2012 until now Professor Farida Fortune Clinical Lead, Consultant in Oral Medicine and Immunology TBC Clinical Nurse Specialist / Centre Manager Nardos Wakjira Lead Dental Nurse Professor Ali Jawad Consultant Rheumatologist Professor Miles Stanford Consultant Ophthalmologist Dr Matthew Buckland Consultant Immunologist Dr Desmond Kidd Consultant Neurologist Dr Steve Higgins - Psychologist Dr Amanda Willis - StR in Oral Medicine Dr Noha Seoudi - StR in Oral Microbiology Dr Bindi Gokhani - Specialty Doctor / Dentist Sheila Bower Business Administration Manager Bridie Sweeney - Administrator Marie Simpson - Secretary Jean Christians Support Coordinator
NHS Complaints Framework NHS New framework Patient Safety Partners. Previous NHS frameworks for complaints has not worked. PHSO new framework. 12/24 months after an event - Not in real time. Investigates very few complaints compared to those reported to the organisation. Should be Real Time Investigations and Obtaining a written witness narrative from carers/relatives/witnesses not a report of your interpretation of what they said. Begin to measure all outcomes costs v benefit and build a feedback system that asks patients and relatives to comment on the treatment they have received.
Research Project Open University- Witness to harm, holding to account: Improving patient , family and colleague witnesses experiences of Fitness to Practise proceedings Improving the experience of witnesses in health and care professional practice proceedings World s first study of this kind Working with 13 UK regulators of health and social care. 30 month project https://www.open.ac.uk/research/news/improving-experience- witnesses-health-and-care-professional-practice-proceedings