Emergency Operations Plan (EOP) Review and Compliance Overview
This comprehensive review covers the objectives of the Emergency Operations Plan (EOP) including healthcare preparedness, CMS Emergency Preparedness Rule, and accreditation requirements. It discusses key aspects to remember when organizing an EOP manual and highlights the impact of CMS compliance on healthcare providers. The content emphasizes the goal of updating the EOP to address system gaps, enhance coordination, and establish consistent emergency preparedness practices across different provider types.
- Emergency Operations Plan
- Healthcare Preparedness
- CMS Compliance
- Emergency Preparedness Rule
- Accreditation
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Emergency Operations Plan (EOP) Review
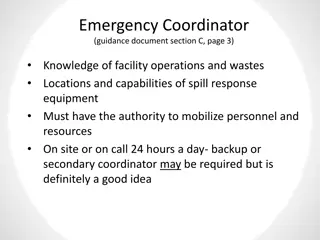
Objectives: Review Healthcare Preparedness Program Structure Recognize Healthcare Preparedness & Response Capabilities Detail the CMS Emergency Preparedness Rule Understand accreditation requirements of the EOP
Things to Remember EOPs Organize into one manual and tab each section Have a limited number of hard copies Have a distribution page Have a changes page Use job aids and checklists that coincide with each specific type of incident identified in the risk assessment It should be specific to your facility
CMS Emergency Preparedness Rule Overview and impacts
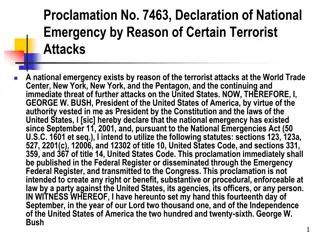
CMS Compliance Centers for Medicare & Medicaid Services Conditions of Participation (CoPs) and Conditions for Coverage (CfCs) Health and safety regulations Must be met by all Medicare & Medicaid- participating providers and suppliers. Conditions of reimbursement. The EP Rule s purpose is to: Enhance patient safety during an emergency. Enhance healthcare delivery system resilience.
Who is Impacted? Hospitals Intermediate Care Facilities for Intellectually Disabled Religious Nonmedical Health Care Institutions Home Health Agencies Ambulatory Surgical Centers Outpatient Rehab Critical Access Hospitals Hospices Community Mental Health Centers Psychiatric Residential Treatment Facilities Organ Procurement Organizations All-Inclusive Care for the Elderly (PACE) Rural Health Clinics Transplant Centers End Stage Renal Disease Facilities (Dialysis) Long-Term Care (LTC) Facilities
Goal of EP Update Goal of EP Rule Updates: Address healthcare system gaps. Establish consistent emergency preparedness practices across provider & supplier types. Encourage emergency coordination with region & localities.
Four Requirements Apply to All Provider Types
Risk Assessment & Planning Perform risk assessment using an all-hazards approach. Update annually Risk Assessment to include: Care-related emergencies Equipment and Power Failures Communications interruption, including cyberattacks Loss of all/portion of facility or clinical supplies
Risk Assessment, contd. Develop an emergency plan (updated annually) based on the risk assessment. Key elements: Integrated approach- demonstrate ability to address a broad range of hazards. Addresses shelter-in-place/evacuation Business Continuity & Continuity of Care Collaboration with local/regional/state Emergency Mgmt
Policies & Procedures Develop and implement policies and procedures based on the emergency plan and risk assessment. Policies and procedures must address a range of issues including subsistence needs, evacuation plans, procedures for sheltering in place, mutual aid, patient tracking, medical records, etc. Review and update policies and procedures at least annually.
Assumptions Scenarios Single Facility / Isolated Incident (e.g., Fire, Loss of Emergency Power); Single Facility / Local or Area-wide Incident (e.g., Flooding, Ice Storm, Blizzard); Multiple Facility / Statewide or Regional Incident (e.g., Derecho, Hurricane, Tornado).
Incident Management Background CMS EP Rule Internal Emergency Operations Plan National Preparedness System NIMS Nursing Home Incident Command System LTC-MAP Pg. 7-Internal Emergency Operations Plan
Communication Plan Develop a communication plan that complies with both Federal and State laws. Coordinate patient care within the facility, across health care providers, and with emergency management systems. Review and update plan annually.
Communication Plan, contd. Communications Plan must include: Names/Contact info for stakeholders Primary and alternate means of communicating with stakeholders Process/method for sharing medical records and patient information Process for sharing logistical information such as census, needs, and ability to provide assistance to other facilities.
Training & Testing Program Develop and maintain training and testing programs. Facilities encouraged by CMS to engage local/state EM and health care coalitions to meet this requirement. Training program must include: Initial EP training for new & existing staff, individuals providing services on behalf of facility, and volunteers (consistent with their expected roles). Documentation of training activities Provision of annual update training for all staff.
Training & Testing Program Testing (Exercise) Program must include: Annual exercises to test emergency plans Tabletop Exercise (recommends HSEEP, but not required) Community-based Full-Scale Exercise If full-scale with community not possible, document why and conduct individual facility-based exercise. Facility is exempt from full-scale requirement for 1 year if an actual or man-made emergency results in activation of the emergency plan. Documentation required
Facility-Specific Rules Outpatient providers not required to have policies on provision of subsistence needs. Home Health Agencies and hospices required to inform local EMA of patients in need of evacuation during an emergency. Long-Term Care and residential Psych facilities must share emergency plan information with residents & their family members.
Facility-Specific Rules Outpatient providers not required to have policies on provision of subsistence needs. Home Health Agencies and hospices required to inform local EMA of patients in need of evacuation during an emergency. Long-Term Care and residential Psych facilities must share emergency plan information with residents & their family members. Additional requirements for Emergency Power and Standby Systems for hospitals, critical access hospitals, and Long-Term Care
Expectations for Emergency Management NOT local EMA s responsibility to ensure or assist with successful certification. Local EM s CAN expect entities to contact them about: Obtaining copies of jurisdictional HVA or THIRA Plan/policy integration Engaging in training/exercise opportunities Basic information on emergency preparedness and healthcare system preparedness
Expectations for Emergency Management EMAs are not required to certify plans! EMAs (collaborate with CVEMA?) should develop a standard level of service for requesting facilities: Standard One-Pager Set platform for relationships and collaboration despite limited resources Encourage collaboration with Public Health and Healthcare Coalition
Questions? Pete Svoboda MVP Coordinator Central Virginia Healthcare Coalition pete.svoboda@central-region.org RHCC 24/7 Activation: 1-800-276-0683