Understanding Psychiatric Challenges in Homeless Populations
This module sheds light on the prevalence of psychiatric disorders among homeless individuals compared to non-homeless, emphasizing issues like suicidal ideation and attempts. It also highlights the lack of psychiatry-specific training in addressing homelessness, and the potential benefits of street psychiatry services in providing essential care to the homeless population.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Slides from Dr. Sheryl Fleisch MODULE 5 What follows are the supplemental slides for module 5. Slides created by Sheryl Fleisch, M.D. Assistant Professor of Psychiatry and Behavioral Sciences at Vanderbilt Director of the Psychosomatic Medicine Fellowship Program and Medical Director of Vanderbilt Street Psychiatry and Homeless Health Services at Vanderbilt Module 5 Slide 1
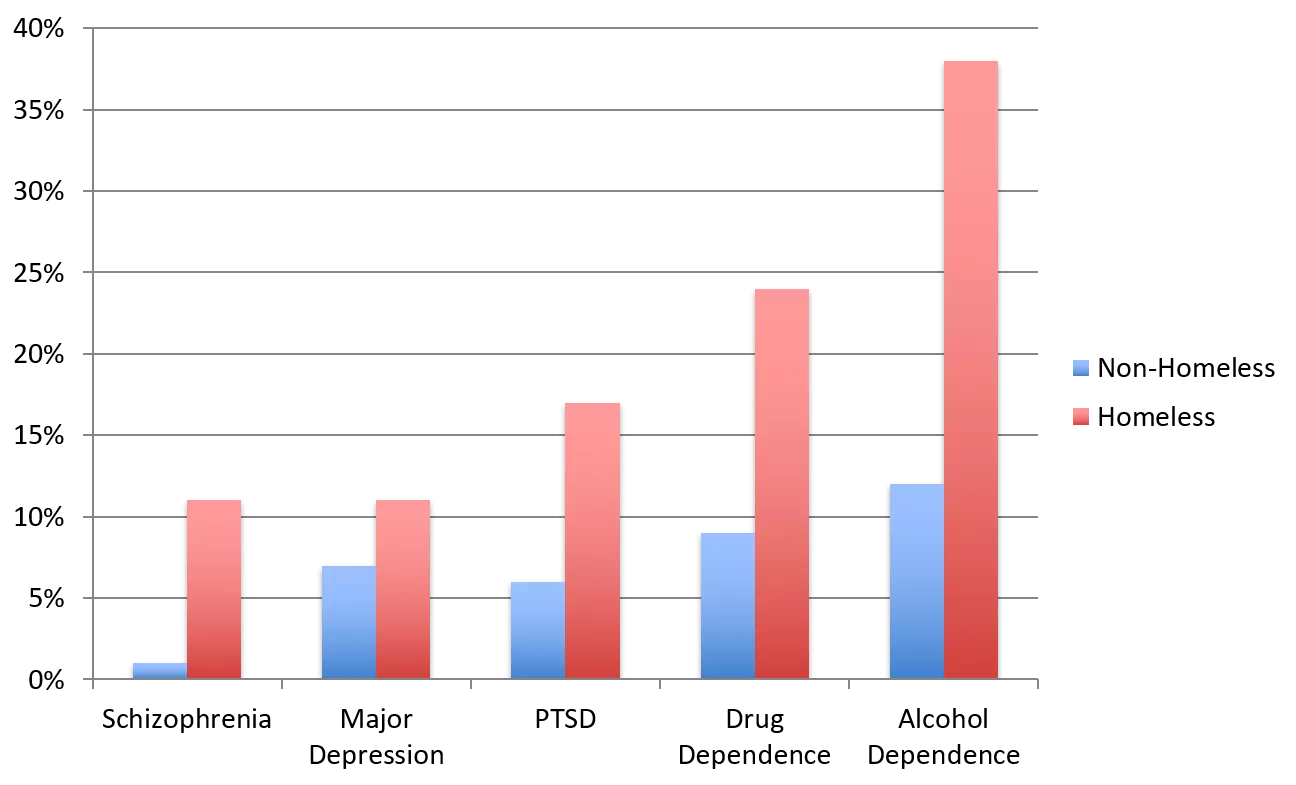
Psychiatric Disorders in Homeless vs. Non-Homeless 40% 35% 30% 25% 20% Non-Homeless Homeless 15% 10% 5% 0% Schizophrenia Major Depression PTSD Drug Alcohol Dependence Dependence Fazel 2008, SAMSHA 2012, NIMH Module 5 Slide 2
Suicidal Ideation and Homelessness Desai et al, 7,224 homeless persons with mental illness ~2/3 had suicidal ideation ~1/2 reporting history of suicide attempt Desai R, Liu-Mares W, Dausey D, et al. Suicidal Ideation and Suicide Attempts in a Sample of Homeless People with Mental Illness. J Nerv Ment Dis. 2003;191(6):363- 171. Module 5 Slide 3
Psychiatry-Specific Training in Homelessness Psychiatry residency programs curricula, through didactics or clinical rotations addressing homelessness (2004 survey) Only 60% offer it Only 11% require it McQuistion HL, Ranz JM, Gillig PM. A Survey of American Psychiatric Residency Programs Concerning Education in Homelessness. Academic Psychiatry. 2004;28(2):116-21. Module 5 Slide 4
Street Psychiatry Underdeveloped field, normally seen as an adjunct to the street medicine model Approximately 85 national/international street medicine programs (20 countries, 35 U.S.) with an unknown number of psychiatrists who assist on the streets Advantages of active psychiatric care on the streets Assist in engaging homeless in their medical care Street therapy Provide psychiatric medications on the street Assist in connecting with case management Provide SSI/SSDI evaluations Module 5 Slide 5
Street Preventive Care Background 40yo man vomiting 56yo man intoxicated 41yo man psychotic Medical Issue Chronic pancreatitis Frostbite of toes Sprained ankle Propane heater, socks, toe warmers; therapy ACE bandage, new shoes, Advil; therapy Intervention Water, crackers, Zofran Refuses Hospital due to social anxiety Refuses Hospital due to poor insight Hospital Overuse due to Psychosis Why Street Clinic F/U 1 week; No hospitalization Outcome F/U 1 week; No ER visit F/U 1 week; No 911 call Module 5 Slide 6
Vanderbilt Street Psychiatry Outpatient street consultation clinic (Partner w/ local non-profit) July 2014: clinic began Jan 2015: mobile pharmacy Jan 2016: billing clinic Jan 2017: injectables available July 2017: expand to young adult shelter Teaching Psychiatry Residents (year-long rotation) Medical Students (day-long experience) Other professionals (day-long experience) SW, RN, pharmacy, hospital leadership Module 5 Slide 7
Vanderbilt Street Psychiatry Cited as favorite elective among medical students I believe that I ll never forget that day I spent with your team, and I believe it will be one of those formative medical school experiences that will have an influence on how I practice and view medicine During my time on the clerkships it can, at times, feel like it s all about spending time on computers, watching screens, and administrative work; however, I think this experience truly was a window to see the core of what medicine is: people reaching out to other people to provide help, comfort, reassurance, truth, dignity, and so many other things Module 5 Slide 8
Click Here to Access an Article from Vanderbilt Medicine about the Program Module 5 Slide 9
Identify Needs in Your Community Understand your city s poverty rate (https://www.census.gov/topics/income-poverty/poverty.html) Review Point In Count Data for your city (https://www.hudexchange.info/programs/hdx/guides/pit-hic/#general-pit- guides-and-tools) Appreciate Fair Market Rent in your community (https://www.huduser.gov/portal/datasets/fmr.html) Learn about Medicare and Medicaid coverage (https://www.cms.gov/) Learn about the hospitals servicing your community and the demographics of patients they serve Read about free and sliding scale mental health, physical health, dental, and other clinics in your city Module 5 Slide 10
How Can You Take Action! Volunteer Free Clinic Shelter Food Bank Teach Formal Medical Student Didactics On the Fly When you graduate Accept patients who are uninsured or on medicaid Module 5 Slide 11
Forming Your Own Initiatives Ideas Building a Street Psychiatry Program Starting a Psychiatry Clinic at a local shelter Developing a clothing closet for discharge needs Gas card/bus card program for transportation to and from appointments Indigent medication programming Homeless education for medical students Module 5 Slide 12
Strategies for Success Obtain Internal and External Champions (if necessary) Align Incentives and Know Your Audience Ex: you want to provide psychiatric care on street CEO may want $$ and program director may want to count towards ACGME requirement Determine Collaboration Structure How will you work with your partners? Is there money exchange? Who will supervise? Method to Prove Your Effectiveness Why should your champions support you? Are you saving money, innovating a teaching method, developing a unique rotation? Doing a good thing, may not be good enough! You will need to prove value. Module 5 Slide 13
Institutional Challenges in Treating Homeless Persons Hospital-wide pressure to discharge if non-acute to open up acute beds Traditional outpatient procedures may not be accomplished due to chronic homelessness leading to non-acute events becoming acute Hospital is writing off cost for unfunded patients No additional compensation for social complexity Risk of physicians spending less time on socially complex patients due to incentive model Lack of affordable citywide transit Patients are unable to attend regularly scheduled outpatient appts resulting to more frequent ER visits No actual place to go; lack of housing navigation services Lack of shelters, respite facilities, SNFs that will accept homeless persons directly from the hospital Module 5 Slide 14
Pearls to Better Accommodate Homeless Persons in the Hospital Setting Start with a homelessness history Where are you physically staying now? Where did you stay before where you are staying now? Before that? This will help you understand a person s situation and they will appreciate you are interested! Ask about Ability to afford medications Insurance status, income per month, how $$ is currently being used Ability to afford and utilize transportation Likelihood of following up with outpatient appointments Access to cell phone and best way to be reached if no phone Barriers to care previously and currently Module 5 Slide 15