Management of Uncomplicated Sore Throat with a New Quick PCR Point-of-Care Test
A prospective study explored the utility of a high-sensitivity PCR test for Group A Streptococci in managing uncomplicated sore throats. Findings showed reduced antibiotic prescribing rates and targeted treatment, emphasizing the importance of testing patients and prescribing antibiotics based on test results. Recommendations include testing all patients or only those meeting specific criteria, with different approaches based on the presence of rheumatic fever concerns. Senior doctors were more likely to prescribe antibiotics despite negative test results.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
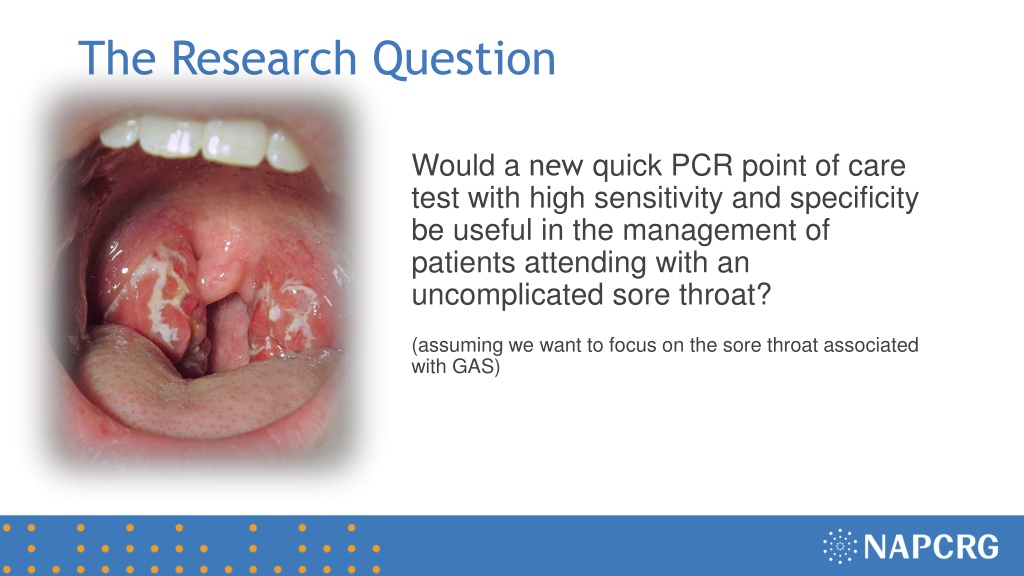
The Research Question Would a new quick PCR point of care test with high sensitivity and specificity be useful in the management of patients attending with an uncomplicated sore throat? (assuming we want to focus on the sore throat associated with GAS)
Research Design and Method Prospective cross-sectional study including consecutive patients attending primary health care for an acute uncomplicated sore throat Patients symptom and signs was registered as well as doctors management before and after a point of care PCR test to detect group A streptococci Descriptive statistics of management before and after PCR test Descriptive statistics of management if any of a set of different guidelines had been adhered to Multivariable logistic regression to identify factors associated with antibiotic prescribing despite a negative PCR test
What the Research Found 283 patients included (interquartile age range 11-36 years). Group A Streptococci (GAS) were found in 31% The PCR test reduced antibiotic prescribing from 46% to 41% and prescribing became more targeted to those ill from GAS. No patients ill from GAS would be left without antibiotics if all are tested and antibiotics prescribed if test is positive. Adhering to the US and Swedish guidelines of only prescribing antibiotics in case of 3-4 Centor criteria and a positive test would have resulted in the lowest prescribing rate. Senior doctors were much more prone to prescribe antibiotics if a PCR test was negative compared to junior doctors.
What this means for Clinical Practice If rheumatic fever is a concern test all patients with a sore throat and prescribe antibiotics to all having a positive test for presence of group A streptococci. If rheumatic fever is not a concern only test patients with 3-4 Centor criteria and only prescribe antibiotics if a test is positive for presence of group A streptococci. Do not test those having 0-2 Centor scores. (Patients with known immunodeficiency may have to be managed in other ways)







![Preventing Influenza at [Name of Critical Access Hospital]](/thumb/233818/preventing-influenza-at-name-of-critical-access-hospital.jpg)