Understanding Protein Energy Malnutrition (PEM): Signs, Symptoms, and Treatment
Protein Energy Malnutrition (PEM) is a serious nutritional disorder resulting from a deficiency of macronutrients, energy, and protein in the diet. This article explores the different types of PEM, focusing on clinical forms like Kwashiorkor, Marasmus, and Marasmic Kwashiorkor. Detailed descriptions of symptoms such as edema, growth failure, mental changes, hair and skin changes, as well as other signs commonly associated with PEM are discussed. The article also delves into the treatment and management of PEM, emphasizing the importance of proper nutrition and intervention strategies in vulnerable populations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
E- CLASS ASSIGNMENT BSC FOOD SCIENCE AND NUTRITION (SEM-IV) TOPIC : PEM (SIGN AND SYMPTOMS, TREATMENT) Subject : Com m unity N utrition
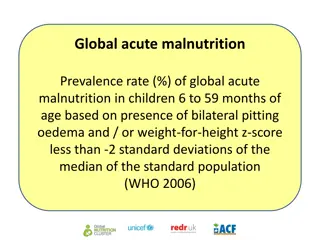
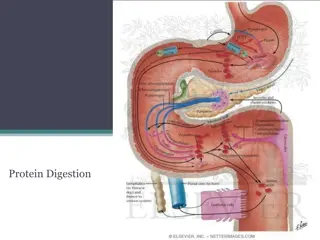
PROTEIN ENERGY MALNUTRITION Protein Energy Malnutrition (PEM) is the deficiency of macronutrients or energy and protein in the diet. It is a nutritional disorder, which affects all the segments of population like children, women and adult males particularly from the backward and downtrodden communities. Different Types of PEM Clinical forms o Kwashiorkor o Marasmus o Marasmic kwashiorkor Sub-clinical forms Underweight Wasting Stunting
KWASHIORKOR Kwashiorkor is an African word, meaning a "disease of the displaced child", who is deprived of adequate nutrition. Mostly in children between the ages of 1 and 3 years, when they are completely weaned (taken off the breast). The three essential manifestations or signs of kwashiorkor are: 1. Oedema (swelling of feet) 2. Growth failure, and 3. Mental changes.
CLINICAL SIGNS OF KWASHIORKOR IN DETAIL Oedema: accumulation of fluid in the tissues. Usually begins with a slight swelling in feet gradually spreading up the legs. Later, hands and face may also have oedema. Poor growth: Growth retardation is the earliest manifestation. The child will be lighter and shorter than its normal peers of same age and weigh about 80% or less of their normal peers. Sometimes, in cases of gross swelling, the body weight may be relatively higher. The child will also be wasted (thinner). The child's arms and legs will appear thin as a result of wasting. Mental changes: kwashiorkor child has no interest in the surrounding. The child will also be irritable and prefers to stay at one place and in one position.
OTHER SIGNS WHICH MAY BE PRESENT ARE Hair changes: In kwashiorkor, the hair loses its healthy sheen and becomes silkier and thinner. It takes coppery red colour (referred to as 'discoloured hairy). You could easily pluck small tufts of hair without causing any pain (referred to as easy pluck ability) just by passing your hands through the hair. Skin changes: In many cases, dermatosis (changes in skin) is seen. Such changes are common in areas of friction. Moon face: The cheeks may seem swollen with fluid or fatty tissue and often be slightly sagging. Micronutrient deficiencies: Almost all the children manifest anaemia (due to iron deficiency) of some degree. Eye signs of vitamin A' deficiency are also common. Manifestations of vitamin B complex deficiency are also noted in many cases.
MARASMUS Marasmus is common in children below the age of 2 years. The marasmic children are so weak that they may not have even energy to cry, which most often is barely audible. The child is extremely wasted with very little subcutaneous fat with the skin hanging loosely particularly over the buttocks. Oedema is absent and there are no skin and hair changes. However, frequent diarrhoeal episodes leading to dehydration and micronutrient deficiencies of vitamin A, iron and B-complex are common.
Signs and Symptoms of Marasmus Extreme muscle wasting - "skin and bones" Loose and hanging skin folds Old man's or monkey faces Absolute weakness
MARASMIC KWASHIORKOR Sometimes, in areas where PEM is common, malnourished children exhibit the features of both kwashiorkor and marasmus. Such changes could occur during the transition from one form of severe PEM to another. These children will have extreme wasting of different degrees (representing marasmus) and also oedema (a sign of kwashiorkor). They may also man Signs and symptoms of Marasmic Kwashiorkor Extreme muscle wasting - "skin and bones" Loose and hanging skin folds Old man's or monkey's face Absolute weakness Oedema
BIOCHEMICAL SIGNS SPECIFIC TO PEM Biochemical Changes Marasmus Kwashiorkor Serum albumin Normal or slightly decreased low Urinary urea per g of the creatinine Normal or decreased low Urinary Hydroxyproline Index low low Serum free amino acid ratio Normal Elevated Anaemia May be observed Common iron and folate deficiency may be associated Reduced enzymatic activity Pancreatic secretions Reduced enzymatic activity
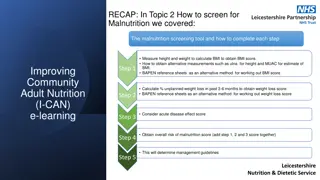
TREATMENT Diet Treatment of cases of kwashiorkor or marasmus involves mainly providing appropriate nutrition support. The child should receive a diet that provides adequate amounts of energy and protein. Both of these are required in larger quantities than normal. The child should be given the following concentrations: Energy : 170 - 200 kcal per kg of body weight Protein : 3 - 4 g/kg of body weight Vitamin and mineral supplements All cases of severe PEM require multivitamin preparation to meet the increased demands during recovery. Iron (60 mg) and folic acid (100 mg) may be given daily to correct anaemia.
Oral rehydration Since diarrhoea is very common in severe PEM, correction of dehydration is the first step in the treatment. Home made (salt-sugar mixture) or commercial oral rehydration solution (ORS) can be administered to correct dehydration. Intravenous fluids are required only in severe dehydration. Control of infections and infestations Appropriate antibiotics should be started immediately since infections are the immediate cause of death in many children. Children with intestinal infestations Like giardiasis and ascariasis should be treated. "prevention is better than cure". So it becomes extremely important that we make sincere efforts to prevent and control PEM
SUPPLEMENTARY FEEDING PROGRAMMES Food supplementation programmes have a very important role to play to combat malnutrition. The aim of these supplementary feeding programmes is to improve the nutritional status of vulnerable groups through distribution of food supplements. Following supplementary feeding programmes : 1. National Programme of Nutritional Support to Primary Education (Mid Day Meal Programme) 2. Special Nutrition Programme 3. Pradhan Mantri's Gramodaya Yojana (PMGY) 4. Balwadi Feeding Programme 5. Composite Nutrition Programme, and 6. Applied nutrition programme
MID DAY MEAL PROGRAMME The National Programme of Nutritional Support to Primary Education commonly known as Mid Day Meals Scheme was launched in August, 1995 The mid day meal programme is one of the most important ongoing feeding programmes organized by the Department of Education not only to improve nutritional status of school children but also to attract poor children to school. Objectives The programme is intended to give a boost to universalization of primary education by increasing enrolment, retention and attendance and simultaneously impacting upon nutritional status of students in primary classes.
SPECIAL NUTRITION PROGRAMME The Special Nutrition Programme was launched by the Central Social Welfare Board (CSWD) in 1970-71. The aim of the programme was to provide supplementary nutrition to children, pregnant women and nursing mothers belonging to the weaker sections of the society. The main component of the programme was food supplementation. The supplement consisted of 300 Kcal and 10 g protein for children and 500 Kcal and 25 g protein for Pregnant- lactating women. Feeding of the beneficiaries was undertaken for 300 days a year. In addition to supplementary feeding, the scheme also included periodic health check ups for the beneficiaries.
PRADHAN MANTRI'S GRAMODAYA YOJANA (PMGY) In order to achieve the objective of sustainable human development at the village level, a new initiative in the form of Pradhan Mantri's Gramodaya Yojana (PMGY) has been introduced in the Annual Plan 2000-01. Schemes related to health, nutrition, education, drinking water, housing and rural roads are undertaken within this programme The PMGY has two components: Prograrmmes for rural connectivity with 50 percent allocation, and other programmes of primary health, primary education, rural shelter, rural drinking water and nutrition with the remaining 50 percent allocation.
BALWADI FEEDING PROGRAMME Like the Special Nutrition Programme , the Balwadi Feeding Programme was also launched in 1970-71. Although the Special Nutrition Programme is no longer in operation, the Balwadi Feeding Programme remains one of the ongoing programmes - implemented through the voluntary organizations. The beneficiaries of the programme include preschool children attending the Balwadi. The services provided under the programme are supplementary feeding, regular health check-ups, immunization, habit formation and socialization through games and recreation. The nutrition programme also has an educative value as it brings together several children of the same age and is expected toinculcate good habits and help children develop taste for different types of foods.
COMPOSITE NUTRITION PROGRAMME The Composite Nutrition Programme was a feeding programme launched by the Department of Community Development, with the main objective of providing nutrition education to the masses. The core of the programme was nutrition education and its particular application through demonstration feeding. The programme had five components: 1. Nutrition education through mahila mandals 2. Encouragement of economic activities of mahila mandals , 3. Strengthening 'the supervisory machinery for women's programme 4. Training of associate women workers, and 5. Demonstration feeding
APPLIED NUTRITION PROGRAMME The Applied Nutrition Programme was one of the first national nutrition programmes launched in 1963 through the Community Development Department, Aimed at improving the nutrition of lactating and pregnant women and children. The programme was developed 'to educate rural people about how they can increase and improve their food supply through their own efforts'. The main objectives of the programme were: 1. To encourage production of body-building foods (such as eggs, fish, milk etc.) and protective foods (such as vegetables, fruits), and 2. To provide nutrition education, so as to promote consumption of the body-building protective foods by mothers and children.