Derbyshire Advanced Clinical Practitioners Three-Year Strategy (2021-2024)
Collaboratively created by the Derbyshire Clinical Practice Group, the three-year strategy aims to enhance the development and contribution of Advanced Clinical Practitioners (ACPs) in delivering safe and effective patient care. It focuses on addressing current barriers in education, capability, and career advancement for ACPs through logic models and detailed roadmaps for improvement. Key areas include standardizing education, promoting interprofessional learning, and aligning curricula with workforce needs.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
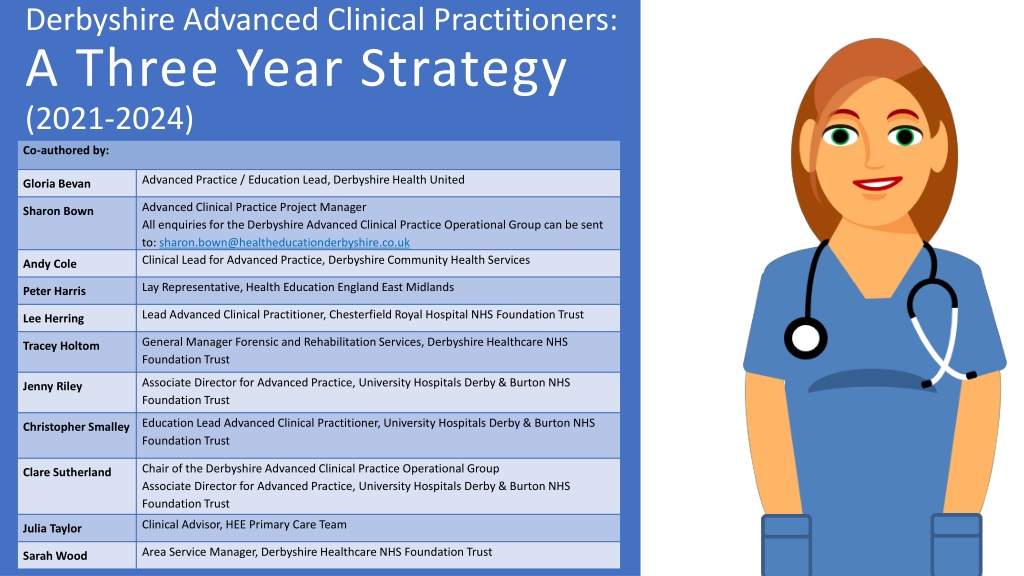
Derbyshire Advanced Clinical Practitioners: A Three Year Strategy (2021-2024) Co-authored by: Advanced Practice / Education Lead, Derbyshire Health United Gloria Bevan Advanced Clinical Practice Project Manager All enquiries for the Derbyshire Advanced Clinical Practice Operational Group can be sent to: sharon.bown@healtheducationderbyshire.co.uk Clinical Lead for Advanced Practice, Derbyshire Community Health Services Sharon Bown Andy Cole Lay Representative, Health Education England East Midlands Peter Harris Lead Advanced Clinical Practitioner, Chesterfield Royal Hospital NHS Foundation Trust Lee Herring General Manager Forensic and Rehabilitation Services, Derbyshire Healthcare NHS Foundation Trust Tracey Holtom Associate Director for Advanced Practice, University Hospitals Derby & Burton NHS Foundation Trust Jenny Riley Education Lead Advanced Clinical Practitioner, University Hospitals Derby & Burton NHS Foundation Trust Christopher Smalley Chair of the Derbyshire Advanced Clinical Practice Operational Group Associate Director for Advanced Practice, University Hospitals Derby & Burton NHS Foundation Trust Clare Sutherland Clinical Advisor, HEE Primary Care Team Julia Taylor Area Service Manager, Derbyshire Healthcare NHS Foundation Trust Sarah Wood
Introduction This strategy has been created by members of the Derbyshire Collaborative Advanced Clinical Practice Group. Our vision is to create confident, capable and adaptable Advanced Clinical Practitioners (ACPs) who are able and willing to contribute to system wide delivery of safe effective care for patients, their relatives and carers. Logic models are used to highlight current issues hindering the education, capability and career development for ACPs and to identify the inputs, or activities required to achieve the desired improvement goals. A three-year roadmap for each workstream is provided in addition to potential measures of success.
Assumptions and External Factors Facilitators Barriers Protected time for education, supervision and supported professional activities can be agreed across all settings for ACPs Staff & employers are motivated to support change Partner organisations work collaboratively Competitive market Limited sphere of influence within Primary Care Variable understanding of advanced practice by employers Limited funds available to support innovation
Improving access to and standardisation of education Inequality and variability in education provision, curricula and access to learning for ACPs Current education provision focuses on clinical capabilities at the expense of leadership, research & education pillars Current educational provision is focused on the development and qualification of ACPs in training SITUATION: ACTIVITIES OUTCOMES: GOAL: Develop a structured review process for all new curriculum and credentials across Derbyshire Embed interprofessional learning across the system Identify, develop & evaluate educational resources available to the system across all 4 pillars Strengthen links with relevant education providers Encourage utilisation of the apprenticeship levy Curricula meet workforce requirements Learning is shared across professions Access to relevant educational opportunities Transparent feedback for learner experience Appropriate utilisation of funds Improved governance of supervision Collaborative working that demonstrates improved access and reduced variability in the provision of education across four pillars
Increase Capability for ACPs The process of reviewing capability of trainee ACPs is inconsistent and reliant on a paper-based system Application of the title Advanced Clinical Practitioner is inconsistent, resulting in confusion for patients and employers Standards for support and supervision of trainees are not explicit, resulting in variation across the system SITUATION: OUTCOMES: ACTIVITIES: GOAL: Agree and commit to robust Annual Review of Progress (ARCP) governance process Implement ePortfolio for all ACPs Create a local directory of ACPs and their progress with education/training Develop a multi-professional model of supervision for trainee ACPs across the Derbyshire ICS Provide training for assessors & supervisors Explore strategies for supporting ACPs in difficulty Standardised Annual Review of Progress process Improved ability to share and review portfolio of evidence Regular access to appropriate support and supervision Support process for ACPs in difficulty A supported, capable and accountable ACP workforce which enhances patient safety outcomes
Improve Career Development for ACPs Limited collaboration between partner organisations to support ACP development Limited opportunities to participate in research, education and leadership activities. Lack of system flexibility due to local reliance on ACPs as workforce solution. SITUATION: ACTIVITIES: GOAL: OUTCOMES: Provide intra and inter- organisational rotational posts Improve annual appraisal process Introduce job planning Create clinical academic and leadership opportunities for ACPs Strengthen pathway from post- registration to consultant level practice ACPs have improved variety of experiences across the system Continuous professional development needs are identified ACPs are engaged in wider supporting professional activities Increased career opportunities that maximise the retention of qualified ACPs within the system
Improving access to and standardisation of education Three Year Plan 3 1 2 Year 1 Year 2 Year 3 Develop new educational resources & promote on website which can be used across all clinical settings and professions Establish a community of practice for ACP Educators Three yearly review of approved curricula. Identify existing ACP educational opportunities Process of agreement for approved Derbyshire curricula implemented and approved curricula circulated to trainees. Link up ACP educators from across the settings Add educational opportunities to the ACP website Promote across all settings
Increase Capability Three Year Plan 2 1 3 Year 1 Year 2 Year 3 ARCP system and process agreed and implemented Eportfolio launched Derbyshire ACP database created and maintained Model of supervision agreed systemwide Provision of supervisor training Establish ACP supervisor forum Engage with the Regional Faculty leads to explore requirements of accreditation for ARCP. Mapping of Health Education England credentials to specialities creating career pathways post qualification. Accreditation of the Derbyshire ARCP process. Evaluation of the standards for supervision and supervisors Evaluation of any new support roles implemented as part of the strategy to ensure fit for purpose and providing value for money.
Improve Career Development Three Year Plan 1 2 3 Year 1 Year 2 Year 3 Write business plan for ACP fellowships Launch revised appraisal process and job plans for all ACPs Develop business case for cross-organisational rotational ACP posts Recruit to cross- organisational ACP posts Establish ACP leadership / clinical academic roles Evaluate appraisal and job planning process Scope existing rotational opportunities Establish standards for annual appraisal and job planning for Derbyshire ACPs Create development framework standards for qualified ACPs
Measures - Education Evidence of.. Activity/outcome/goal/ assumptions? Measure How will you measure it Rationale Why choose this measure? Issues or limitations Curricula meet workforce requirements Feedback from ACP leads Success at ARCP Includes subjective & objective Multiple curricula Learning is shared across professions Increased opportunities for Interprofessional education and learning Measure of increased educational resources available & attendance Time to access opportunities Access to relevant educational opportunities Measure of increased educational resources available. Increased attendance Measure of increased educational resources available & attendance Cost data from various sources, varying time-frames. Transparent feedback for learner experience Gather evaluation of opportunities Can collate the evaluation into feedback Will need admin support to undertake and collate Appropriate utilisation of funds Numbers of trained ACPs Numbers accessing the apprenticeship levy Need a process for primary care to access levy Improved governance of supervision Record ACP supervisors on a directory so we have robust data - Attracting good numbers of trained supervisors Once there is a directory it s easier to have governance for the county
Measures - Capability Evidence of.. Activity/outcome/goal/ assumptions? Measure How will you measure it? Rationale Why choose this measure? Issues or limitations Standardised Annual Review of Progress process Guidelines produced for annual review process and final sign off Ensures a standardised approach to sign off across Derbyshire. Multiple curricula will necessitate training in all curricula and requirements for completion. Percentage of portfolios reviewed Provides a standard for local ARCP Lack of an eportfolio makes sharing of portfolios across assessors challenging. Improved ability to share and review workplace based assessment Successful roll out of eportfolio to all ACPs & supervisors Facilitates system wide review of portfolios for assessment. Facilitates supervision from across the system. No eportfolio currently. Would need to ensure that any eportfolio invested in can be shared with supervisors and panel chairs. Regular access to appropriate support and supervision Evidence of timetabled supervision in portfolios and job plans Trainee feedback Increased number of standard outcomes at first submission ARCP Ensures all ACPs both in training and post qualification have on going developmental support. Limited numbers of supervisors in practice. Limited funding to support ACP supervision. Support process for ACPs in difficulty All ACPs have access to support and know how to access this. Ensure that ACPs can be supported during periods of difficulty. No current ACP wellbeing and support in place, will require investment.
Measures - Career Progression Evidence of.. Activity/outcome/goal/ assumptions? Measure How will you measure it? Rationale Why choose this measure? Issues or limitations ACPs have improved variety of experiences across the system Staff Surveys Better career opportunities should increase job satisfaction. Data collected nationally could facilitate bench-marking Individual groups of staff may not be identified through national surveys Continuous professional development (CPD) needs are identified Proportion of annual appraisals completed Annual appraisals offer opportunity to identify CPD needs Variable ways of recording completion of appraisals Training Needs Analysis ACPs are engaged in wider supporting professional activities Proportion of ACPs with Job Plans Job plans indicate proportion of time spent on clinical and non- clinical activities Currently no way of identifying roles shared across organisations Proportion of ACPs undertaking additional roles, for example supervisor, mentor, research, service improvement, clinical academic