Managing Diabetes, Hypertension, and Cholesterol: Overview of Treatment Guidelines
The guidelines outline step-by-step management strategies for borderline diabetes, hypertension, and cholesterol. For diabetes, lifestyle changes are first recommended, followed by medication if necessary. Hypertension management starts with diet and exercise, then progresses to medication if needed. Cholesterol levels are categorized as low, medium, or medium-high risk. Regular monitoring, patient education, and lifestyle modifications are key components for achieving good control. Referral to a hospital is advised if conditions are not adequately managed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
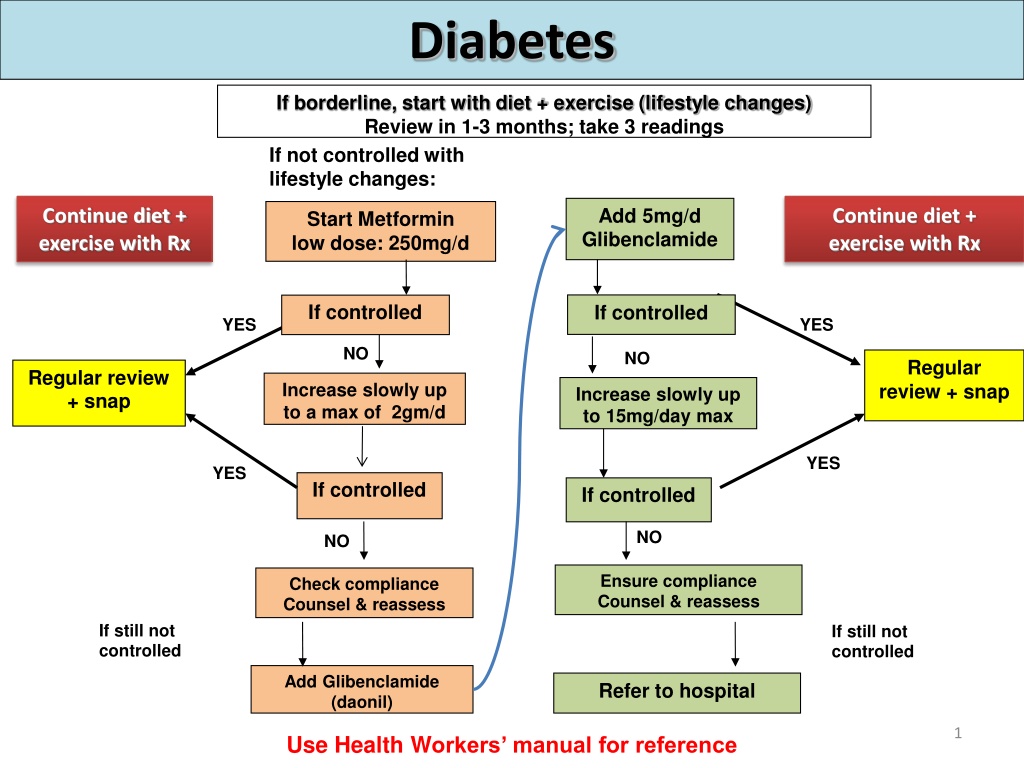
Diabetes If borderline, start with diet + exercise (lifestyle changes) Review in 1-3 months; take 3 readings If not controlled with lifestyle changes: Add 5mg/d Glibenclamide Continue diet + exercise with Rx Continue diet + exercise with Rx Start Metformin low dose: 250mg/d If controlled If controlled YES YES NO NO Regular review + snap Regular review + snap Increase slowly up to a max of 2gm/d Increase slowly up to 15mg/day max YES YES If controlled If controlled NO NO Ensure compliance Counsel & reassess Check compliance Counsel & reassess If still not controlled If still not controlled Add Glibenclamide (daonil) Refer to hospital 1 Use Health Workers manual for reference
Diabetes Diabetes aim for good control Start Rx if: Fasting blood sugar is constantly > 7mmol/L , OR Random blood sugar is constantly > 11mmol/L For good control of diabetes, aim for: Fasting BSL of < 7.0 mmol/L, OR Random BSL of <10.0 mmol/L Readings of >10 indicate poor control In addition to Rx 1. Do a cardio-vascular risk assessment using the CVD risk chart. 2. Explain to the patient what it means. 3. Educate and counsel on lifestyle changes + compliance 4. Follow up regularly and aim for good control 5. Refer to hospital if not controlled Note: For a pregnant woman with diabetes, refer to hospital
Hypertension If borderline, start with diet + exercise (lifestyle change) Review in 1 to 3months; take series of readings Start Rx Hydrochorothiazide (Esidrex 12.5mg/d) Lifestyle change SNAP Lifestyle change SNAP Regular review SNAP Is BP under control? YES NO YES Check compliance Patient education Increase 25mg/d Is BP under control? NO Add Enalapril 2.5mg/d Slowly increase up to a max of 10mg bd If still uncontrolled, refer SNAP - smoking, nutrition, alcohol & physical activities 3
Hypertension aim for good control Consider medication if: Systolic BP >140 Systolic BP >135 if they also have diabetes Do risk assessment using risk chart to determine when to start Rx For good control of hypertension, aim for: Systolic BP of below 140 SBP of below 135, if patient also has diabetes In addition to Rx: 1. Do a cardio-vascular risk assessment using the CVD risk chart. 2. Explain to the patient what the colour means. 3. Educate and counsel on lifestyle changes + compliance 4. Follow up regularly and aim for good control 5. Refer to hospital if not controlled For a pregnant woman with high blood pressure, refer to hospital If BP very high (SBP >200) or patient has symptoms, give nifedipine S/L, observe and refer.
Cholesterol Medium Medium risk risk Low risk Low risk High risk High risk Risk - Risk - Risk - Risk - Green Green Risk - yellow yellow Risk - Red Red No Rx with No Rx with No Rx with statins statins Review 3yrs No Rx with statins statins Review 2yrs Start statins if cholesterol Start statins if cholesterol above 7mmol/L above 7mmol/L Review 5yrs Review 2yrs In all situations regardless of risk level, must do lifestyle changes
Asthma and Chronic Obstructive Pulmonary Disease (COPD) Attend to SOB and relieve symptoms Discharge Rx Prednisone 40mg daily for 3 days only + inhalers Steroids: Ventolin Nebuliser Repeat if needed every 15-30min +/- Prednisone 40mg x 3d Or Hydrocortisone 100mg IV stat If not improving: - Admit and refer - Discharge with long- term Rx Becotide 2 puffs BD daily + If SOB settles: Go home with Rx and follow up Ventolin 2puffs as required Add antibiotics if yellow sputum + fever. Give Amoxycilline or Doxicycline Prevent recurrent attacks by avoiding all sources of smoke cigarettes, tobacco, 2nd hand smoking, cooking fire, bush fire, allergens (peanuts, shellfish). This requires patient education. 6
Asthma and COPD Add Steroids if patient comes with: Repeated attacks in recent weeks or past month Poor response to ventolin nebuliser after 3-4 repeats Dose Prednisone 40mg stat, then 40mg daily x 3days Hydrocortisone 100mg IV stat (if cannot swallow prednisone), followed by prednisone 40mg daily x 3days If patient not responding, admit to ward. If good response, observe and send home with good patient education on the 2 types of puffers. If there is no ventolin nebuliser, use ventolin puffers and spacers: Add 20 puffs into spacer and breath into mouth piece at normal breathing rate, in and out 20 times.