Regulatory Advisory Panel Meeting and Roll Call Participants
The Regulatory Advisory Panel meeting held on October 29, 2020, at 1:00 p.m. featured a roll call of participants from various organizations and agencies. Attendees were muted to ensure an orderly meeting, and members of the media were directed to contact Rebekah Allen. Key organizations included AARP, Alzheimer's Association, and Capital Caring Health among others. Workgroup members from different entities also took part in the meeting, representing a diverse range of healthcare sectors. The roll call included professionals from the Office of Licensure and Certification, the Department of Health, and the Richmond & Henrico Health Districts.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
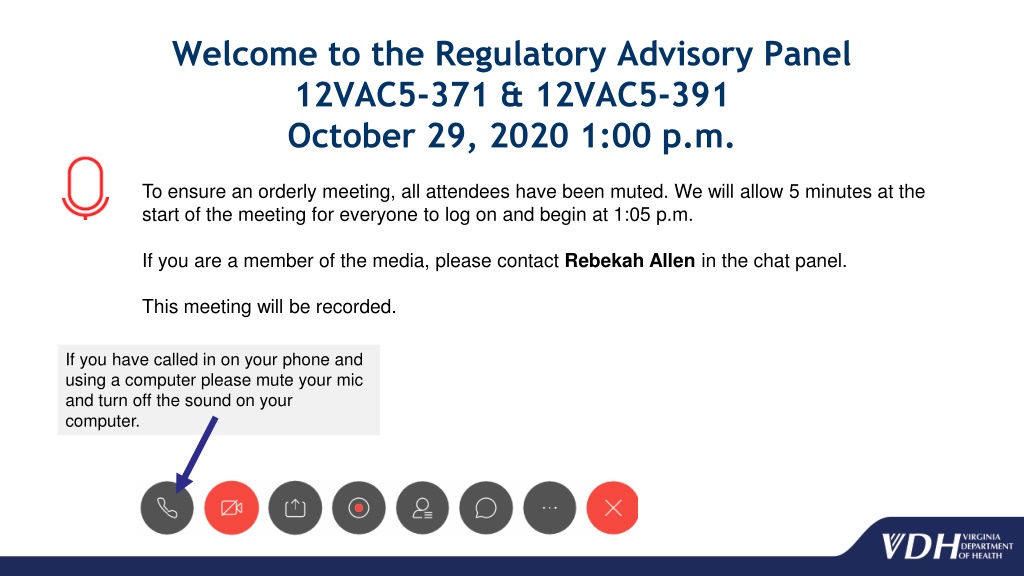
Welcome to the Regulatory Advisory Panel 12VAC5-371 & 12VAC5-391 October 29, 2020 1:00 p.m. To ensure an orderly meeting, all attendees have been muted. We will allow 5 minutes at the start of the meeting for everyone to log on and begin at 1:05 p.m. If you are a member of the media, please contact Rebekah Allen in the chat panel. This meeting will be recorded. If you have called in on your phone and using a computer please mute your mic and turn off the sound on your computer.
Roll Call Name Organization or Agency David Abraham (designee Rebecca Moralez) Beth Sholom Village Melissa Andrews LeadingAge Virginia John Burns (designee Will Blackwell) Westminster Canterbury Richmond William Coleman (designee Colleen Lobb) The Virginia Home Ronald J. Cottrell Hospice of the Piedmont David DeBiasi AARP Carrie Davis Covenant Woods Joann Dawson Bedford Hospice House Morris Funk Beth Sholom Lifecare Community Carter Harrison Alzheimer's Association, Virginia Chapters Tracey Jennings Centra Richard Kennedy Blue Ridge Hospice House Tom Koutsoumpas (designee Matthew Kestenbaum) Capital Caring Health
Roll Call Work Group Member Organization or Agency Joani Latimer State Long Term Care Ombudsman Vivienne McDaniel Virginia Nurses Association Kathryn J. Morrison Sentara Hospice House Dana Parsons LeadingAge Virginia April Payne Virginia Health Care Association | Virginia Center for Assisted Living Greg Storer Williamsburg Landing Marcia Tetterton Virginia Association for Home Care and Hospice Community Hospice House, Bon Secours Board of Long-Term Care Administrators, Department of Health Professions Virginia Lifecare Planning The Center for Elder Law & Estate Planning Carla Thompson Corie E. Tillman Wolf Veronica Williams Mindy Wyttenbach-Lindsey Virginia Association for Hospices and Palliative Care
Roll Call Name Organization or Agency Rebekah E. Allen Office of Licensure and Certification, Department of Health Kimberly F. Beazley Office of Licensure and Certification, Department of Health Kristin Collins Office of Epidemiology, Department of Health Joseph Hilbert Governmental and Regulatory Affairs, Department of Health Sarah File Lineberger Office of Epidemiology, Department of Health Ruth Morrison Richmond & Henrico Health Districts, Department of Health Sara Noble Richmond & Henrico Health Districts, Department of Health Brenden Rivenbark Governmental and Regulatory Affairs, Department of Health
Regulatory Advisory Panel - Agenda Public Comment Period Charge of the Regulatory Advisory Panel Rebekah Allen, Senior Policy Analyst Office of Licensure and Certification Ms. Allen Defining Compassionate Care Discussion and Recommendations on Facility Visitation Obligations during Technology Failures, Service Interruptions, or Documented Emergencies Discussion and Recommendations on Transparency and Communicating Visitation Protocols Ms. Allen and Regulatory Advisory Panel Members Ms. Allen and Regulatory Advisory Panel Members Recommendations of the Regulatory Advisory Panel Ms. Allen and Regulatory Advisory Panel Members
Public Comment Period Written public comments were received and distributed to the RAP Written comments should be sent to Rebekah.Allen@vdh.virginia.gov There is a two minute time limit for each person to speak. We will be calling from the list generated through registration. After the 2 minute public comment limit is reached we will let you complete the sentence and will mute you and move on to the next attendee. We will call the name of the person on list and also the name of the person is next on the list.
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I Amends Va. Code 32.1-127(B) to read: 28. During a public health emergency related to COVID-19, shall require each nursing home and certified nursing facility to establish a protocol to allow each patient to receive visits, consistent with guidance from the Centers for Disease Control and Prevention and as directed by the Centers for Medicare and Medicaid Services and the Board. Such protocol shall include provisions describing
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I (i) the conditions, including conditions related to the presence of COVID- 19 in the nursing home, certified nursing facility, and community, under which in-person visits will be allowed and under which in-person visits will not be allowed and visits will be required to be virtual; (ii) the requirements with which in-person visitors will be required to comply to protect the health and safety of the patients and staff of the nursing home or certified nursing facility; (iii) the types of technology, including interactive audio or video technology, and the staff support necessary to ensure visits are provided as required by this subdivision; and (iv) the steps the nursing home or certified nursing facility will take in the event of a technology failure, service interruption, or documented emergency that prevents visits from occurring as required by this subdivision
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I Such protocol shall also include (a) a statement of the frequency with which visits, including virtual and in-person, where appropriate, will be allowed, which shall be at least once every 10 calendar days for each patient; (b) a provision authorizing a patient or the patient's personal representative to waive or limit visitation, provided that such waiver or limitation is included in the patient's health record; and (c) a requirement that each nursing home and certified nursing facility publish on its website or communicate to each patient or the patient's authorized representative, in writing or via electronic means, the nursing home's or certified nursing facility's plan for providing visits to patients as required by this subdivision
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I Amends Va. Code 32.1-162.5 to read: C. Regulations for hospices shall require each hospice facility to establish a protocol to allow each patient to receive visits, consistent with guidance from the Centers for Disease Control and Prevention and as directed by the Centers for Medicare and Medicaid Services and the Board, during a public health emergency related to COVID-19. Such protocol shall include provisions describing
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I (i) the conditions, including conditions related to the presence of COVID- 19 in the hospice facility and community, under which in-person visits will be allowed and under which in-person visits will not be allowed and visits will be required to be virtual; (ii) the requirements with which in-person visitors will be required to comply to protect the health and safety of patients and staff of the hospice facility; (iii) the types of technology, including interactive audio or video technology, and the staff support necessary to ensure visits are provided as required by this subsection; and (iv) the steps the hospice facility will take in the event of a technology failure, service interruption, or documented emergency that prevents visits from occurring as required by this subsection
Chapters 10 and 11 of the 2020 Acts of Assembly, Special Session I Such protocol shall also include (a) a statement of the frequency with which visits, including virtual and in-person, where appropriate, will be allowed, which shall be at least once every 10 calendar days for each patient; (b) a provision authorizing a patient or the patient's personal representative to waive or limit visitation, provided that such waiver or limitation is included in the patient's health record; and (c) a requirement that each hospice facility publish on its website or communicate to patients or their personal representatives, in writing or via electronic means, the hospice facility's plan for providing visits to patients as required by this subsection
Defining Compassionate Care RAP previously discussed whether to create a special category of visitor for family and/or friends Assistance with ADLs (common feature of other states implementation) raises liability concerns for facilities and may raise licensing concerns for the individual providing the care RAP discussed whether to define compassionate care in such a way as to include these types of visitors Compassionate care circumstances listed in CMS memo QSO-20-39-NH Assistance in maintaining or improving the quality of care or quality of life for a resident or patient
DISCUSSION AND RECOMMENDATIONS ON FACILITY VISITATION OBLIGATIONS DURING TECHNOLOGY FAILURES, SERVICE INTERRUPTIONS, OR DOCUMENTED EMERGENCIES
Questions to Consider What constitutes an emergency? What specific documentation should a facility maintain? For virtual visitation, what information should a facility communicate to scheduled visitors? How should this information be communicated? For in-person visitation, what information should a facility communicate to scheduled visitors? How should this information be communicated? What information should a facility proactively share with its regulator about technology failures, service interruptions, or documented emergencies?
DISCUSSION AND RECOMMENDATIONS ON TRANSPARENCY AND COMMUNICATING VISITATION PROTOCOLS
South Carolina Public Health Order No. COVID-19-5 Licensed nursing homes and community residential care facilities required to submit a weekly report that states: Whether they are permitting visitation If visitation is not permitted, the reason(s) for that decision The number of residents receiving visitors in the last 7 days Reports due 5PM each Monday, through DHEC s website Facilities must immediately report (by email): Human resource challenges in completing requirements Information technology challenges in completing requirements
Questions to Consider In communicating its visitation plans, what minimum information should a facility provide residents and patients? How to schedule visits? Days and times for scheduled visits? Maximum intervals between visits? How the facility will implement outdoor in-person, indoor in-person, and virtual visitation? Health and safety requirements for visitors? Compassionate care exceptions? Should facilities communication of its visitation plans include daily updates? If yes, how are those updates communicated? What documentation should facilities maintain to demonstrate this communication?
RECOMMENDATIONS OF REGULATORY ADVISORY PANEL
Recommendations 1. As a general matter, nursing homes, certified nursing facilities, and hospice facilities are expected to provide in-person visitation. 2. Nursing homes, certified nursing facilities, and hospice facilities have the discretion to determine if in-person visitation will occur indoors, outdoors, or a mix of the two. 3. If the COVID-19 county positivity rate is greater than 10%, nursing homes and certified nursing facilities may not provide in-person indoor visitation except for compassionate care visits. 4. If the COVID-19 county positivity rate is equal to or less than 10%, nursing homes and certified nursing facilities may consider the health district rate of COVID-19- Like Illness visits to the emergency department and the COVID-19 county positivity rate of adjacent localities when determining whether to permit in- person indoor visitation.
Recommendations (cont.) 5. If there is an outbreak of infectious disease including COVID-19, influenza, and norovirus, nursing homes and certified nursing facilities may not provide in-person indoor visitation except for compassionate care visits if so directed by the local health department. 6. There are no community- or facility-level conditions for hospice facilities that indicate the need to hold virtual visitation only. 7. Visitation in nursing homes, certified nursing facilities, and hospice facilities may be limited to virtual visitation on a case-by-case basis for specific visitors who do not meet health and safety requirements.
Recommendations (cont.) 8. The following professional entrants into nursing homes, certified nursing facilities, and hospice facilities should be screened for COVID-19 before entry: 8.1 State Health Commissioner or his designee (i.e. Medical Facilities Inspectors) 8.2 Representatives of the State Long-Term Care Ombudsman 8.3 Representatives of protection and advocacy systems 8.4 Assistants to effective communication if not otherwise available on site 8.5 Representatives of Adult Protective Services and Child Protective Services 8.6 Members of the clergy and representatives of pastoral care 8.7 Guardians ad litem; court-appointed attorneys; and attorneys retained by the resident or resident s guardian or responsible person or party
Recommendations (cont.) 9. The health care workers who are not employees, but provide direct care to residents or patients should be tested for COVID-19 before entry into nursing homes, certified nursing facilities, and hospice facilities. 9.1 This includes attending physicians or nurse practitioners with autonomous practice privileges, employees of licensed hospices, and employees of licensed home care organizations or certified home health agencies. 9.2 This requirement does not apply to emergency medical services (EMS) personnel entering the facility to provide emergency care to residents or patients. 10. Representatives of the State Long-Term Care Ombudsman, representatives of protection and advocacy systems, and representatives of Adult Protective Services and Child Protective Services must have immediate access to residents and patients. 10.1 In-person access is to be provided unless the representative fails the COVID-19 screening. 10.2 If the representative fails the COVID-19 screening, the nursing home, certified nursing facility, or hospice facility must provide immediate virtual access.
Recommendations (cont.) 11. The family or friends of residents or patients entering into nursing homes, certified nursing facilities, and hospice facilities should be screened for COVID-19 before entry. 11.1 Compassionate care should be defined to include the circumstances listed in CMS memo QSO-20-39-NH and to include assistance in maintaining or improving the quality of care or quality of life for a resident or patient. 11.2 Nursing homes, certified nursing facilities, and hospice facilities should maintain in- person visitation logs that document for each visitor: 11.2.1 Name 11.2.2 Contact information (phone and email address, if available) 11.2.3 Date and time of visit 11.2.4 Which resident or patient the visitor is there to see 11.3 Nursing homes, certified nursing facilities, and hospice facilities may condition in- person visitation on a visitor s agreement to contact the facility if the visitor receives a positive COVID-19 test within 14 number of days of their visit.
Recommendations (cont.) 12. Nursing homes, certified nursing facilities, and hospice facilities should adhere to the most recent guidance from the U.S. Centers for Disease Control and Prevention and as directed by the U.S. Centers for Medicare and Medicaid Services and the State Board of Health. 12.1 Nursing homes, certified nursing facilities, and hospice facilities should instruct visitors on the relevant portions of their infection prevention and control policies and procedures prior to the visitor meeting with a patient or resident. 12.2 Nursing homes, certified nursing facilities, and hospice facilities may refuse entry to a visitor who refuses to abide by infection prevention and control policies and procedures. 13. Nursing homes, certified nursing facilities, and hospice facilities should retain discretion to determine what minimum staff are needed to facilitate outdoor in-person visitation, indoor in-person visitation, and virtual visitation. 13.1 Nursing homes, certified nursing facilities, and hospice facilities must specify what minimum levels of staff are needed for visitation in their facility in their written visitation policies and procedures.
Recommendations (cont.) 14. Nursing homes, certified nursing facilities, and hospice facilities may require visitors to schedule visitation. 14.1 The requirement to schedule visits does not apply compassionate care visitation. 14.2 Nursing homes, certified nursing facilities, and hospice facilities should reserve visitation capacity to accommodate unanticipated compassionate care visitation or other unscheduled visitation needs. 15. Nursing homes, certified nursing facilities, and hospice facilities should be sanitizing shared virtual visitation equipment before each use and after each use, using cleaning products recommended by the equipment manufacturer. 16. Nursing homes, certified nursing facilities, and hospice facilities must offer visitation to each resident, patient, or the resident or patient s guardian or responsible person or party at least once every ten calendar days. 16.1 The offer of visitation and the response to the offer must be documented in the resident s clinical record (in the case of nursing homes and certified nursing facilities) or in the patient s medical record (in the case of hospice facilities).
ADDITIONAL RECOMMENDATIONS FROM TODAY S DISCUSSION