Syncope: Diagnostic Algorithm and Management Overview
Syncope is defined as a transient loss of consciousness due to cerebral hypoperfusion, with rapid onset and complete recovery. It poses risks of falls, trauma, and sudden death but is mostly benign in young individuals. Initial evaluation includes a thorough history, physical exam, and ECG. Classification includes orthostatic hypotension, reflex, cardiac, and other causes. Guidelines emphasize the importance of diagnosis and management strategies. www.escardio.org offers detailed guidelines for reference.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Syncope diagnostic algorithm and management MUDr. Jakub Hon k Kardiologick klinika, 2.LF UK a FN Motol, Praha
Definition of syncope Syncope is a T-LOC due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery. T-LOC all cases of transient loss of consciousness regardless of the pathophysiological mechanism Spontaneous complete recovery Transient loss of consciousness Global cerebral hypoperfusion = circulatory cause Rapid onset Short duration ESC Guidelines for the diagnosis and management of syncope (version 2009): Moya et al. Eur Heart J, 2009.
Significance, epidemiology Risk of fall and trauma A warning signal of sudden death Mostly benign in young A common complaint 3% of emergency visits A fraction of patients see a doctor Bimodal age distribution
Prognosis, significance of syncope management and diagnostics Soteriades et al. N Eng J Med, 2003.
www.escardio.org/guidelines www.escardio.org/guidelines
Classification of syncope Syncope from ortostatic hypotension Reflex syncope Cardiac syncope Vasovagal Situational Carotid sinus hypersensitivity Atypical forms Primary ANF Secondary ANF Drug-induced Volume depletion Arrhythmia as a cause Structural heart disease
www.escardio.org/guidelines www.escardio.org/guidelines
Initial diagnostic work-up A thorough history What preceded syncope, prodromes, eyewitness report, symptoms after syncope Personal and family history, medication, recurrent syncope? Physical exam BP supine and standing 5 min. supine, 1st and 3rd min. standing ECG
Initial evaluation key questions Is it syncope? Syncope? Was diagnosis made? Diagnosis? Is there a high-risk profile for casrdiovascular diseases or high sudden-death risk? Risk?
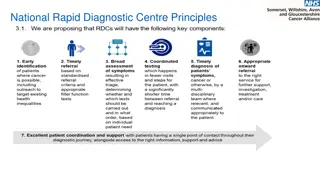
Initial evaluation Suspected syncope Syncope NO Diagnosis made Diagnosis uncertain Consider other diagnosis Low risk, recurrent Low-risk, sporadic High-risk Admitt, diagnose, treat Diagnose, treat? No further work-up
www.escardio.org/guidelines www.escardio.org/guidelines
Initial evaluation Risk startification Structural heart disease CHD (previous MI), heart failure, aortic stenosis, HCM Clinical or ECG signs suggestive of arrhytmic etiology Syncope while supine, exercising, palpitations Family history of sudden death Bifascicular block, nsVT, susp. SSS, preexcitation, QTc, Brugada, susp. ARVC Age >40 + recurrent syncope (50% arrhythmia) Severe comorbidities Anemia, ion dysbalance
Further evaluation Diagnostic methods Carotid massage Pause > 3s, BP drop > 50 mmHg Unknown cause in pts. > 40 yrs Tilt test Reflex syncope - cardioinhibitory, vasodepresoric and mixed reaction X ortostatic hypotension Indicated in suspected reflex syncope, unknown etiology, susp. OH, difdg. of falls, pseudosyncope
Further evaluation Diagnostic methods ECG monitoring In-hospital monitoring High-risk pts. Holter ECG (24h, 48h, 7d) frequent syncope/presyncope Implantable/external loop recorder (ILR) Recurrent syncope of unknown etiology, therapy- resistant epilepsy, susp. arrhytmic cause Arrhythmia during syncope or occurrence of severe arrhythmia make diagnosis, syncope with no ECG changes rule out arrhythmic cause
Further evaluation Diagnostic methods Electrophysiological exam Specific indications, high suspicion not confirmed non-invasively Echocardiography Risk stratification, structural heart disease Stress test Psychiatric evaluation Neurological evaluation
www.escardio.org/guidelines www.escardio.org/guidelines
Take home messages Not every LOC is a syncope Thorough history is the cornerstone Initial evaluation makes diagnosis 25- 40%, risk-stratification in the rest There is plenty of diagnostic methos, use them wisely
Therapy Indications for permanent pacing SSS + ECG correlated symptoms SSS + abnormal CSNRT Asymptomatic pauses >6s (SSS/AVB) AVB II Mobitz II, AVB III BBB + abnormal HV conduction Alternating BBB BBB + unexplained syncope risk/ILR Reflex cardio-inhibitory ultimum refugium Syncope due to hypersensitive carotid sinus