Analysis of Prehospital Resuscitation: Insights from Ukraine's Clinical Protocols
Clinical and statistical analysis of Emergency Medical Dispatch (EMD) teams in Ternopil, Ukraine, from 2018 to 2020 revealed key trends in prehospital resuscitation. The study assessed arrival times, mortality rates, resuscitation measures, and successful outcomes. Challenges and recommendations were identified based on the data analysis.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
PREHOSPITAL RESUSCITATION: PROBLEMS, SUCCESSES AND RECOMMENDATIONS ACCORDING TO MODERN CLINICAL PROTOCOLS IN UKRAINE Ya.M.Kitsak, O.H.Tys, R.M.Liakhovych, M. Ya. Djus
Resuscitation - a set of measures aimed at restoring impaired or lost vital functions of the body (cardiopulmonary and cerebral functions). severely
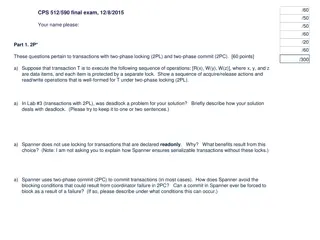
MATERIALS AND METHODS We conducted a clinical and statistical analysis for 2018- 2020 of the EMD teams of Ternopil, who went on calls to the victims who were in a state of clinical death. The study was based on cover letters, departure cards, which reflect the time of receipt of the call, the time of arrival to the victim, the presence (absence) of home care, comprehensive (including successful) resuscitation measures conducted by the EMD team, the statement of biological death . The quality and complexity of the diagnosis was assessed by comparative analysis of diagnoses made by emergency physicians.
Table 1. Absolute mortality, home care and travel time of emergency crews to patients with sudden circulatory arrest Year 2018 2019 2020 The total number of analyzed cases 407 409 495 Arrival time up to 10 minutes 378 391 459 Arrival time after 10 minutes 29 18 36 The number of deaths before the arrival of the EMT 335 333 408 The number of deaths after the arrival of the EMT 54 62 72 Number of deaths with injuries that are incompatible with life and in the terminal stages of oncology, hemopathology, etc. 299 234 307 Number of cases of home care before the arrival of the EMT 9 13 17 - from them in the first 5 minutes. 2 3 6 - of them after 5 minutes 7 10 11
Table 2. Analysis of resuscitation measures performed by EMD teams according to the type of sudden cessation of blood circulation and the number of successful resuscitations YEAR 2018 2019 2020 Number of resuscitation measures performed 40 65 79 Number of patients with ECG diagnosis such as sudden cessation of blood circulation Number of diagnosed ventricular fibrillation / ventricular tachycardia Number of diagnosed asystoles 34 59 65 27 34 47 17 15 18 Number of successful resuscitations 3 3 7 - of diagnosed ventricular fibrillation / ventricular tachycardia - of diagnosed asystoles 2 3 5 1 0 2
Table 3. Adherence to modern protocols of sudden cardiac arrest in ventricular fibrillation and asystole Year 2018 2019 2020 The total number of performed cardiopulmonary resuscitation Timely execution of precardiac stroke 40 65 79 4 4 9 Timely defibrillation 19 25 33 Timely provision of venous access 28 41 58 Timely drug therapy 24 37 65
Conclusions In general, the above analysis shows that the dominant factors of high prehospital mortality are the lack or inadequacy of home care, hence the late arrival of doctors, a significant number of chronic incurable patients and fatal injuries that led to irreversible biological death. .
There are also some shortcomings in the organization and quality of pre-medical and hospital care. In particular, it should be noted that some EMD teams are procrastinating in the immediate diagnosis of circulatory arrest (ECG diagnosis), which is a priority at the beginning of resuscitation measures, rather than early intubation or venous access. Also, in a number of cases, a delay in the early defibrillation session as a primary method of eliminating these types of RCTs, as well as incorrect initial and subsequent choice of defibrillation energy were observed in the diagnosis of PF / VT. At registration (A / REA) in almost every second case, a 0.1% solution of atropine was used, although it has been proven that in these types of RCC it is ineffective and therefore should not be used. Tracheal intubation was performed in almost one in four cases, but in most cases it was performed at an early stage of SLMR with long-term cessation of resuscitation (average 30-40 s) and delay in rhythm identification and defibrillation.
In appropriate to present our own vision of the algorithm for providing pre-hospital medical care to victims who are in a state of clinical death. connection with the above data, we consider it The most important task of providing emergency medical care in patients with sudden cardiac arrest is to restore vital functions of the body, so the diagnosis of their condition by the ABC system is mandatory (A - patency of the upper respiratory tract, B - assessment of respiration C - assessment of the system blood circulation with the definition (8-10 s) of absolute signs of clinical death). Performing a precardiac stroke in the first 10-20 s from the moment of sudden cardiac arrest on the background of narrow pupils and the finding on the ECG of ventricular fibrillation / ventricular tachycardia with a defibrillator not ready to work.
Immediate cardiopulmonary resuscitation in a ratio of 30/2, with a chest compression rate of at least 120 per 1 minute. Early defibrillation (if indicated) whenever technically possible, regardless of the duration of clinical death and the number of cycles of cardiopulmonary resuscitation. Refusal of early intubation of the trachea in favor of rapid ECG- diagnosis such as sudden cardiac arrest, defibrillation with the use of alternative methods of artificial ventilation. Refusal of atropine as a universal remedy for circulatory arrest by the mechanism of asystole or electromechanical dissociation without a pulse. Refusal of endotracheal drug administration in favor of intravenous and intraosseous access. Carrying out post-resuscitation therapy according to a certain protocol (including medical hypothermia).
The correct and modern algorithm of cardiopulmonary resuscitation also takes into account the following organizational measures: to begin the necessary treatment without long discussions; anticipate the next stage in the treatment process; prepare for it in advance; work according to the best knowledge and recommendations; be professional (colleagues, family); keep in mind the legal responsibility for providing (not providing) medical care, so follow the clinical protocol as much as possible.