Updates on Maine Health Data Organization (MHDO) Board Meeting Discussions
This content provides insights into the recent discussions and initiatives undertaken by the Maine Health Data Organization (MHDO) Board, including rulemaking timelines for non-claims based payments, an overview of an APCD Federal Grant Opportunity, updates on legislative sessions, and reports on public laws impacting MHDO operations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
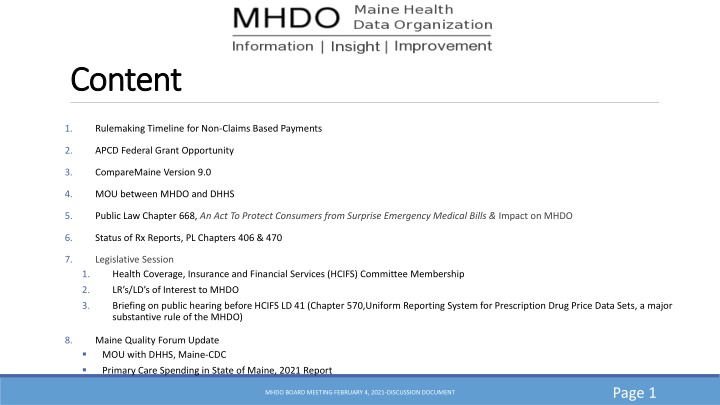
Content Content 1. Rulemaking Timeline for Non-Claims Based Payments 2. APCD Federal Grant Opportunity 3. CompareMaine Version 9.0 4. MOU between MHDO and DHHS 5. Public Law Chapter 668, An Act To Protect Consumers from Surprise Emergency Medical Bills & Impact on MHDO 6. Status of Rx Reports, PL Chapters 406 & 470 7. Legislative Session Health Coverage, Insurance and Financial Services (HCIFS) Committee Membership 1. 2. LR s/LD s of Interest to MHDO 3. Briefing on public hearing before HCIFS LD 41 (Chapter 570,Uniform Reporting System for Prescription Drug Price Data Sets, a major substantive rule of the MHDO) 8. Maine Quality Forum Update MOU with DHHS, Maine-CDC Primary Care Spending in State of Maine, 2021 Report Page 1 MHDO BOARD MEETING FEBRUARY 4, 2021-DISCUSSION DOCUMENT
Timeline for Non-Claims Based Rulemaking New Rule for collecting non-claims based Primary Care Provider Payments Develop proposed rule to collect non-claims based payments from payers specifically those payments made to/for primary care (board unanimously supported in June 2020) Identified Use Case: State s annual report on Primary Care Spending in State of Maine (as required by Public Law Chapter 244) Leverage the structure(s) that currently exists in other states (MA, OR, CO, RI, VT) for the collection of non-claims based payments 2 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued February-April 2021 MHDO meets with key stakeholders (payers, data users and other states experiences collecting non- claims based payments) to gather feedback May-June 2021-MHDO drafts proposed rule Early August-public hearing and proposed rule announced September 2021 MHDO holds public hearing October 2021 MHDO Board reviews public comments and agency responses. Board considers adoption of proposed rule changes 3 MHDO BOARD MEETING FEBRUARY 4, 2021
APCD Federal Grant Opportunity Consolidated Appropriations Act, 2021 SEC. 320B. STATE ALL PAYER CLAIMS DATABASES Summary of section: States can receive up to $2.5 million grant to establish a new APCDs or improve an existing APCD Grant funding is over a three year period (beginning in FY22) To be eligible, states must "ensure uniform data collection" Priority may be given to states that demonstrate cooperation with other state APCDs to facilitate multi-state use Comment: There is a likely role for using the APCD-CDL to satisfy these requirements 4 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued Requirements: When a state accepts grant funding there are several requirements regarding access to APCD data and standard reporting that the APCD must produce. Example: NON-CUSTOMIZED REPORTS. A State All Payer Claims Database that has received a grant under this section shall make available to all authorized users aggregate data sets available through the State All Payer Claims Database, free of charge. WAIVERS. The Secretary may waive the requirements of the subsection of a State All Payer Claims Database to provide access of entities to such database if such State All Payer Claims Database is substantially in compliance with this subsection. 5 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued SEC. 735. STANDARDIZED REPORTING FORMAT Not later than 1 year after the date of enactment of this section, the Secretary shall establish (and periodically update) a standardized reporting format for the voluntary reporting, by group health plans to State All Payer Claims Databases . 6 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued ADVISORY COMMITTEE. 90 days after the date of enactment, the Secretary shall convene an Advisory Committee consisting of 15 members to advise the Secretary regarding the voluntary reporting format for claims data submissions. 7 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued The National Association of Health Data Organizations including the APCD-Council convened the states in January to begin the conversation and sharing of information regarding the provisions and requirements as described in the law. MHDO will continue to participate in both national and regional discussions https://rules.house.gov/sites/democrats.rules.house.gov /files/BILLS-116HR133SA-RCP-116-68.pdf. 8 MHDO BOARD MEETING FEBRUARY 4, 2021
Contract with MHDOs Data Vendor Contract with HSRI terminates November 30, 2022 Federal Grant Opportunity is for a three year period (TBD on application and award timelines. Perhaps award aligns with next federal fiscal year, end of 2021/early 2022) Goal: maximize the federal grant opportunity of $2.5M to enhance our current APCD and minimize disruption for our data submitters (payers and hospitals), data users, and for MHDO s mandated reporting requirements. 9 MHDO BOARD MEETING JUNE 4, 2020
CompareMaine CompareMaine MHDO released version 9.0 of CompareMaine in December 2020. Cost data (defined as payments to providers) updated to represent the time-period April 1, 2019-March 31, 2020 CompareMaine reports: the average payment for 260 health care procedures from 320 facilities by the top 5 commercial payers in the State quality measures including patient survey ratings, preventing serious complications, preventing healthcare associated infections, falls with injury, pressure ulcers and unplanned hospital-wide readmissions Top 25 Rx Reports updated for time-period July 2019-June 2020 Page 10 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued Team is in the process of developing the work plan for CompareMaine V.10.0 Plan to present to the board at the May 6th board meeting Release date December 2021 11 MHDO BOARD MEETING FEBRUARY 4, 2021
MOU Between MHDO and DHHS Purpose: To develop a provider database that will support the Department s Service Locator Tool. Key deliverables include: Use existing MHDO claims and hospital encounter data (includes data from the National Plan and Provider Enumeration System (NPPES)) to gather baseline information to build a provider database that can be used to populate information in the provider service locator tool Collaborate with the provider service locator tool vendor to define a data exchange workflow for exporting data from MHDO databases to the provider service locator tool Collaborate with the provider service locator tool vendor to define a data exchange workflow for receiving data from the provider service locator tool into MHDO databases 12 MHDO BOARD MEETING FEBRUARY 4, 2021
MHDO Provider Directory-Overview The MHDO Provider Database will support the management of healthcare provider information in a directory structure. The data structure will contain person-provider identity information and information about a person provider s relationships to facility providers and health systems. The directory will list healthcare providers classified by provider type, specialties, credentials, demographics and service locations. Nesting of service locations within provider groups and health systems will also be identified. 13 MHDO BOARD MEETING FEBRUARY 4, 2021
Example of Relationships (nesting) in the Example of Relationships (nesting) in the MHDO Database MHDO Database Parent Health System Behavioral Health Group Practice Provider Group Practice Hospital Lab Person-Provider Person Provider Person Provider Behavioral Health Hospital Department Person Provider 14 MHDO BOARD MEETING JUNE 4, 2020
Continued MHDO continues to seek feedback from the broader data user community on the utility of a provider directory and will discuss the status of the Provider Directory at the February data user group meeting. 15 MHDO BOARD MEETING JUNE 4, 2020
Public Law Chapter 668 (LD 2105), An Act To Protect Consumers from Surprise Emergency Medical Bills & Impact on MHDO 2. Requirements. With respect to a surprise bill or a bill for covered emergency services rendered by an out-of-network provider: B. Except as provided for ambulance services in paragraph D, unless the carrier and out-of-network provider agree otherwise, a carrier shall reimburse the out-of- network provider or enrollee, as applicable, for health care services rendered at the average network rate under the enrollee's health care plan as payment in full, unless the carrier and out-of-network provider agree otherwise; and greater of: (1) The carrier's median network rate paid for that health care service by a similar provider in the enrollee's geographic area; and (2) The median network rate paid by all carriers for that health care service by a similar provider in the enrollee's geographic area as determined by the all-payer claims database maintained by the Maine Health Data Organization or, if Maine Health Data Organization claims data is insufficient or otherwise inapplicable, another independent medical claims database; Page 16 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued 4303-E. Dispute resolution process for surprise bills and bills for out-of-network emergency services 1. Independent dispute resolution process 1. C. In determining a reasonable fee for the health care services rendered, an independent dispute resolution entity shall select either the carrier's payment or the out-of-network provider's fee. The independent dispute resolution entity shall determine which amount to select based upon the conditions and factors set forth in this paragraph. In determining the reasonable fee for a health care service, an independent dispute resolution entity shall consider all relevant factors, including: 1.C.(3) The median network rate for the particular health care service performed by a provider in the same or similar specialty, as determined by the all-payer claims database maintained by the Maine Health Data Organization or, if Maine Health Data Organization claims data is insufficient or otherwise inapplicable, another independent medical claims database. If authorized by rule, the superintendent may enter into an agreement to obtain data from an independent medical claims database to carry out the functions of this subparagraph. 17 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued On 2/2 BOI was scheduled to present their analysis of Maine s Surprise Billing law vs the Federal No Surprises law to HCIFS. HCIFS was then scheduled to conduct a public hearing on LD 46, An Act To Further Protect Consumers from Surprise Medical Bills. Due to storm Legislature was closed. Meeting with the BOI, MHDO and Maine Association of Health Plans and Payers occurred 2/3 to discuss how to move forward with the implementation of the current law in light of the data challenges (No in and out of network designation pre January 2021 submissions) and pending legislative action. Next Steps: BOI will discuss internally the recommendation that the payers made regarding the calculation of a median rate until such time that MHDO has the in and out of network designation. 18 MHDO BOARD MEETING FEBRUARY 4, 2021
MHDOs Prescription Drug Data Sets All Payer Claims Data (includes medical and prescription drug claims) Prescription Drug Pricing Component Data from manufacturers, wholesale distributors and pharmacy benefit managers 19 MHDO BOARD MEETING FEBRUARY 4, 2021
Commercial Insurance Pharmacy Paid Amount as a % of Medical Paid, 2009-2019 2009: 23% 2010: 23% (as reported in MHDO s APCD) 2011: 24% 2012: 24% 2013: 27% 2014: 28% 2015: 29% 2016: 39% 2017: 36% 2018: 36% 2019: 35% Source: https://mhdo.maine.gov/tableau/data.cshtml 20
Public Law Chapter 406 An Act to Promote Prescription Drug Price Transparency MHDO must report annually on the following information about prescription drugs, both brand name and generic: The 25 most frequently prescribed drugs in the State The 25 costliest drugs as determined by the total amount spent on those drugs in the State The 25 drugs with the highest year-over-year cost increases as determined by the total amount spent Reports can be found here: https://www.comparemaine.org/?page=rx-costs Data Source: MHDO All Payer Claims Data 21 MHDO BOARD MEETING FEBRUARY 4, 2021
Public Law Chapter 470 An Act to Further Expand Drug Price Transparency MHDO is required to collect data from prescription drug manufacturers, wholesale drug distributors and pharmacy benefit managers (referred to as reporting entities) as described in MHDO Rule Chapter 570 As of December 31, 2020, there are 337 manufacturers, 182 wholesale drug distributors and 32 pharmacy benefit managers registered with MHDO. 22 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued MHDO must produce an annual report beginning November 1, 2020 and submit to Legislature and post on MHDO website: Information on Trends in the Cost of Prescription Drugs Analysis of Manufacturer Prices and Price Increases Major Components of Prescription Drug Pricing Along the Supply Chain Impacts on Insurance Premiums, Cost Sharing, and Other Information the MHDO Determines is Relevant to Providing Greater Consumer Awareness of the Factors Contributing to the Cost of Prescription Drugs in the State of Maine The report may not disclose information attributable to any particular manufacturer, wholesale drug distributor or pharmacy benefits manager. 23 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued Focus of our first annual report is on describing the entities in the pharmaceutical supply chain, their roles and the financial transactions that occur within the supply chain using both MHDO prescription drug claims data and drug pricing component data Discuss feedback from the board on draft report 24 MHDO BOARD MEETING FEBRUARY 4, 2021
130th Maine Legislature 130th Maine Legislature Health Coverage, Insurance and Financial Services Committee Membership Senator Heather Sanborn-Chair Senator Stacy Brenner Senator Trey Stewart Representative Denise Tepler-Chair Representative Poppy Arford Representative Mark Blier Representative Heidi Brooks Representative Jon Connor Representative Richard Evans Representative Kristi Mathieson Representative Gina Melaragno Representative Joshua Morris Representative Tracy Quint Page 25 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued-LRs & LDs MHDO is tracking Resolve, Regarding Legislative Review of Portions of Chapter 570, Uniform Reporting System for Prescription Drug Price Data Sets, a major substantive rule of the MHDO. LD 41 LD 46 An Act to Further Protect Consumers on Surprise Medical Bills LD 120 An Act to Lower Health Care Costs through the establishment of the Office of Affordable Health Care LR 151 An Act To Implement the Attorney General's Recommendations on Data Collection in Order To Eliminate Profiling in Maine LR 541 An Act to Improve Health Care Data Analysis LR 663 An Act to Improve Prescription Information Access LR 740 An Act Regarding Primary Care & Behavioral Health Investment in Cost Savings Resolve, Directing the MHDO to Determine the Best Methods & Definitions to Use in Collecting Data to Better Understand Racial & Thnic Disparities in the Provision of Health Care in Maine. LR 795 LR 1071 LR 1493 LR 1575 An Act to Prevent Excessive Prices for Prescription Drugs An Act to Strengthen Prescription Drug Pricing Transparency An Act to Strengthen Prescription Drug Pricing Transparency 26 MHDO BOARD MEETING FEBRUARY 4, 2021
LD 41 LD 41- -Resolve, Regarding Legislative Review of Portions of Chapter 570, Resolve, Regarding Legislative Review of Portions of Chapter 570, Uniform Reporting System for Prescription Drug Price Data Sets, a major Uniform Reporting System for Prescription Drug Price Data Sets, a major substantive rule of the MHDO substantive rule of the MHDO HCIFS Public Hearing-January 28 No surprises regarding testimony Work Session will be scheduled by the committee to review comments and determine next steps 27 MHDO BOARD MEETING JUNE 4, 2020
Update on 2021 Annual Report: Primary Care Spending in State of Maine (PL Chapter 244) NESCSO released its multi-state report on Primary Care Investment mid January 2021 Primary Care Collaborative (PCC) released a report in early January 2021 on primary care spending trends across the country High level conclusion after reviewing the different reports, is despite using different data sources and difference in methodologies (including exclusion criteria), results are comparable across these reports MQF plans to release the year 2 Primary Care Spending in State of Maine draft report to the MQF Primary Care Advisory Committee by end of this week for review and feedback. Plan is to submit to HCIFS and Commissioner Lambrew (DHHS), as required by statute before end of February. MHDO BOARD MEETING FEBRUARY 4, 2021 28
Continued The purpose of the Memorandum of Agreement between MQF and DHHS, Maine-CDC is to define how MQF will provide the department technical support for Project Firstline. Project Firstline is the CDC s (Federal) new infection control training collaborative, designed to help every frontline healthcare worker gain the knowledge and confidence to stop infections. For the past five years, the Maine Quality Forum, Maine CDC s Healthcare Epidemiology Program, and the University of Southern Maine have worked together to launch a web- based remote training platform for Maine healthcare facilities. It is known as the Maine Infection Prevention Forum (MIPF). With the support of grant funding, the vision for this site is to offer one stop shopping for infection prevention and control training and education for Maine s healthcare community. In collaboration with the Maine-CDC, the Maine Quality Forum through its Cooperative Agreement with the University of Southern Maine, will improve the MIPF and expand the Infection Prevention and Control training programs both in audience and access. 29 MHDO BOARD MEETING FEBRUARY 4, 2021
Continued Summary of key deliverables defined in MOU 1. Conduct high-level learning needs assessments of and provide a summary report on the jurisdiction s healthcare workforce to identify training gaps by setting, describe primary spoken and reading languages, and characterize literacy levels and age in the following healthcare settings: Tier 1: Hospitals, nursing homes, intermediate care facilities for individuals with intellectual disabilities (ICF-IID facilities), and dialysis facilities Tier 2: Ambulatory surgery centers, home health care agencies, and urgent care centers 2. Promote awareness of Project Firstline training modules to targeted frontline healthcare workers, as outlined by the Federal CDC. 3. Utilize the Maine Infection Prevention Forum (MIPF) platform to conduct and convene remote learning capabilities for front-line healthcare workers including tracking of facility uptake by hospitals, nursing homes, ICF-IID facilities, dialysis facilities, ambulatory surgery centers, home health agencies, and urgent care centers. 4. Complete as many secondary activities as time and resources allow: Conduct and convene remote learning capabilities with Assisted Housing facilities and Allied Health students. Create additional modules for the MIPF, including Urinary Tract Infection (UTI) for Maine nursing homes, and updating current MIPF modules. Enhance functionality of the website (e.g., customize reporting engine, improve user interface). 5. Provide requested information to the Department by the 10th of each month for the development and submission of the monthly report to the Federal CDC. 6. Produce workplans, timelines and tracking of status for all deliverables. 7. Meet performance measures as they are established by the Federal CDC for the grant that is the subject of this agreement. 30 MHDO BOARD MEETING FEBRUARY 4, 2021