Understanding Yersinia: Characteristics, Diseases, and Identification
The genus Yersinia includes various species, with Yersinia pestis causing plague and others causing diarrheal diseases. Yersinia organisms are gram-negative rods, often associated with serious infections. Learn about Yersinia pestis, its transmission, identification, morphology, and antigenic structure.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
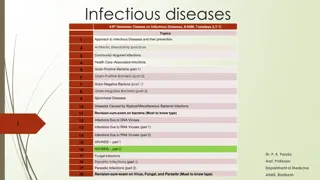
University of Mustanisiriya College of Medicine Department of Microbiology Third stage YERSINIA AND ACINETOBACTER Dr Ali Abdulwahid
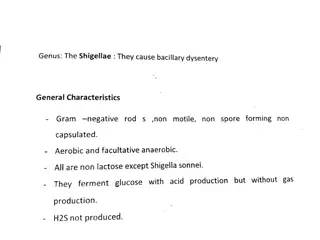
Yersinia The genus Yersinia includes many species: Yersinia pestis the (cause of plague) Yersinia pseudotuberculosis Yersinia enterocolitica The later two species are important causes of human diarrheal diseases There are many other species that are nonpathogenic for humans. The microorganisms are short, pleomorphic gram-negative rods that can exhibit bipolar staining. facultatively anaerobic. catalase positive, oxidase negative Most of the organisms have animals as natural reservoir, and can cause serious infections and diseases for humans.
Yersinia pestis and plague Plague is an infection of wild rodents caused by Yersinia pestis transmitted between rodents and occasionally from rodents to humans by the bites of fleas. Serious infection often results, which in previous centuries produced pandemics of black death with millions of fatalities. The ability of this organism to be transmitted by aerosol and the severity and high mortality associated with pneumonic plague
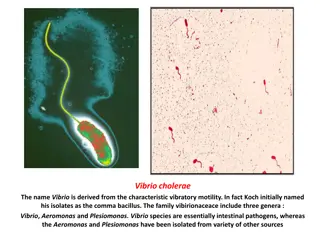
Morphology and identification Gram-negative rods that exhibits striking bipolar staining with special stains such as Giemsa, or methylene blue Nonmotile. Aerobes and facultative anaerobes. Can grow on ordinary media , but it grows well on media containing blood or tissue fluids On nutrient agar, the bacteria form small (0.1-0.2 mm), transparent colonies which can become opaque on continued incubation. It also produces very small colonies on blood agar at 37 C after 24 hours, and they tend to be dark brown due to absorption of e haemin pigment clinical isolates from infected tissue produces gray and viscous colonies, but after passage in several cultures , irregular and rough colonies can be produced .
Blood smear taken from a patient with bubonic. Note the safety pin appearance of Yersinia pestis. U.S. Center for Disease Control - https://www.cdc.gov/ncidod/dvbid/plague/bacterium.htm Diagram of Bipolar appearance of yersinia under microscopic
Antigenic Structure Lipopolysaccharides: as a gram ve bacteria, witch confers endotoxic activity when released. Type III secretion systems: the bacteria have this system that enable them to inject proteins directly into cytoplasm of the host cells. V and W antigens : these antigens are produced by virulent Yersinia and they are: Encoded by genes carried on plasmid They yield the requirement for calcium for growth at 37 C. They inhibit phagocytosis and intracellular killing of the bacillus. Plasminogen-activating protease: This enzyme has temperature-dependent coagulase activity ( at 20 28 C, the temperature of the flea) and fibrinolytic activity (35 37 C, the temperature of the host). This factor facilitate the transmission and spreading of the bacteria from the flea bite injection site to host.
The capsular protein (fraction F1): Production of this protein is plasmid mediated It produced mainly at 37 C and confers antiphagocytic properties. Phospholipase D: encoded by gene carried on the same plasmid carrying gens of fraction F1 This enzyme is required for organism survival in the flea midgut. Iron-scavenging siderophore (yersiniabactin) Exotoxins (murine toxin) There are several exotoxins produced by yersinia Among them , one is lethal for mice in amounts of 1 g. It produces -adrenergic blockade and is cardiotoxic in animals. Its role in human infection is unknown
Pathogenesis and Pathology The commonest vector of plague is the rat flea (Xenopsylla cheopis) During the feeding of flees on the rodent infected with Y. pestis , they ingest the bacteria Then bacteria will multiply in the gut of the flea and forming biofilm. This high growth along with the blood coagulation (due to the coagulase) leads to block the esophagus of the flea. Subsequently, the flea with blocked esophagus want to feed and bites, the aspirated blood enters the esophagus, mixes with the bacteria , and then return back (due to the blockage) into the bite wound. The inoculated organisms may be phagocytosed by macrophages and polymorphonuclear. As the bacteria are able to resist phagocytosis, the pathogens rapidly reach the lymphatics, and an intense hemorrhagic inflammation develops in the enlarged lymph nodes, which may undergo necrosis and become fluctuant.
Y pestis can also reach the bloodstream and spread to the other part of the body . Hemorrhagic and necrotic lesions may develop in all organs. Primary pneumonic plague results from inhalation of infective droplets (usually from a coughing patient), and it is characterized by hemorrhagic consolidation, sepsis, and death.
Clinical Findings The clinical manifestations of plague depend on the route of exposure. Bubonic Plague : After an incubation period of 2 7 days, there will be acute onset of high fever, headache, chillsand weakness. Vomiting and nausea may also develop This is commonly accompanied with greatly enlarged nodes in the neck, groin, or axillae. Septicemic Plague In the early stage of the disease, a sudden onset of fever, Vomiting , nausea, and diarrhea can develop. Later in the course of the infection, disseminated intravascular coagulation leads to hypotension, and renal and cardiac failure. Pneumonic Plague The signs of pneumonia and meningitis can be seen with the course of the disease. the infection acquired by inhalation of the infectious droplets of plague patients. The pathogen multiply intravascularly and can be detected by blood smear Patients often have a fulminant course with chest pain, cough, hemoptysis, and severe respiratory distress.
Diagnostic Laboratory Tests A. Specimens Blood and sputum for culturing aspirates of enlarged lymph nodes and CSF for smear and culturing. Sera: for testing antibody levels . B. Smears The organisms are small gram-negative bacilli they appear either as single cells or as pairs or short chains in clinical samples. Staining with Giemsa, methylene blue: it shows bipolar staining (safety pin appearance) with the two ends of the bacterium are highly intensive with stain and clear region in the middle. Further direct staining : using of fluorescent antibody targeting the capsular F1 antigen of the bacterium
C. Culture Culturing can be done on a wide range of media including : blood agar, chocolate, and MacConkey agar. the organism growth slowly on agar media and require more than 48 hours, but on blood agar plates, positive results can be seen within 24 hours. Cultures can be tentatively identified by biochemical reactions the bacteria are nonmotile. non-lactose fermenter, catalase positive; indole, oxidase, urease negative
D. Serology In none immunized people, a convalescent serum antibody titer of 1:16 or more is an indicator of infection with Y pestis . The results of the serological tests can be confirmed by the rise in the antibody titers in two sequential specimens
Treatment Without effective treatment, the mortality rate of plague disease can reach 50%; and nearly 100% in the case of pneumonic plague The effective antibiotics can involve : streptomycin, aminoglycoside gentamicin and Doxycycline. Drug resistance has rarely been noted in Y. pestis
Epidemiology and Control Plague is an infection of wild rodents that occurs in many parts of the world. the main regions that act as habitats are: India, Southeast Asia (especially Vietnam), Africa, and North and South America. Plague outbreaks among animals which correlated with high mortality rate can occur sporadically, and infection can be transmit from wild to domestic rodents and other animals (eg, rats and cats), and then to humans via flea bites or by direct contact. The control of plague requires surveys of infected animals, vectors, and human contacts If a human case is diagnosed, health authorities must be notified promptly.
All patients with suspected plague should be isolated, especially who with Pneumonic Plague All clinical samples and specimens should be treated with extreme caution. Chemoprophylaxis with doxycycline should be given for contacts of patients with suspected Pneumonic Plague
Yersinia enterocolitica and Yersinia pseudotuberculosis THE ORGANISMS ARE : gram-negative rods urease positive and oxidase negative. Non-lactose-fermenting Grow well at 25 C and are motile at this temperature and lose this feature at 37 C O Serotyping : More than 70 serotypes were described for Y enterocolitica; only isolates from serotypes O:3, O:8, and O:9 cause infection for human . At least six serotypes were described for Y. pseudotuberculosis and isolates of O:1 responsible for most human infections.
. Y. enterocolitica has been isolated from rodents and domestic animals (eg, sheep, cattle, swine, dogs, and cats) and waters contaminated by them. Transmit to humans via contaminated food, drink, or fomites. Y. pseudotuberculosis: occurs in domestic and farm animals and birds, which excrete the organisms in feces. Transmit to humans via ingestion of materials contaminated with animal feces. The infection can rarely transmit from Person-to-person.
Pathogenesis and Clinical Findings Infectious dose: between 108 109 bacterial cells should enter the alimentary tract to cause infection. Within 4 7 days after the entrance of the bacteria , they multiply in the gut mucosa, particularly the ileum resulting in inflammation and ulceration In the early stage of the infection the symptoms can involve: abdominal pain, fever and diarrhea. watery to bloody diarrhea can be resulted due to an enterotoxin effectiveness or to invasion of the mucosa. In rare cases , infection with Yersinia can develop to pneumonia, meningitis, or sepsis.
Y enterocolitica can also transmit from person to person via blood transfusion process as this bacteria have an ability to transmit from asymptomatic donor, and can also multiply at low temperatures of refrigeration.
Treatment diarrhea caused by yersinia are self-limited The organism is susceptible to a wide range of antibiotics include: aminoglycosides, chloramphenicol, tetracycline, trimethoprim third- generation cephalosporins, and fluoroquinolones; sepsis can be treated with third-generation cephalosporins or a fluoroquinolone (that can be in combination with other antimicrobial agents).
Acinetobacter Acinetobacter Gram-negative bacteria that are widely distributed in nature and commonly found in soil and water They are aerobic, oxidase negative and catalase positive. The genus involve many species but the one that is mostly common isolated in clinical lab is Acinetobacter baumanii Other species that can be correlated with human infection are : Acinetobacter lwoffii, Acinetobacter nosocomialis, Acinetobacter peitti and Acinetobacter radioresistance. Such species have been described to colonise human skin and causing infections in immunocompromised people
Morphology and growth The bacteria are usually coccobacillary or coccal in their shape; but sometimes rod-shaped form can be seen Acinetobacter diplococcal forms can also be seen in smear resembling Neisseria , But they can be differentiated by oxidase test : Acinetobacter is oxidase ve while Neisseria is oxidase +ve The organism grow well on culture media used for culturing clinical specimens The majority of Acinetobacter species grow between 20 0C 35 0C , but the clinically important species grow well between 35 0C - 37 0C Some of Acinetobacter baumanii strains can grow at 44 0C
Infections and Pathogenicity of Acinetobacter Acinetobacter are opportunistic pathogens that cause nosocomial infection, especially in immunocompromised people. The organism can be isolated from different environments include : Natural environments : soil, water , animals Hospitals environments: ventilator, catheters and dialysis devises Human: such as skin mucus membranes blood sputum pleural fluid Urine
Infections The bacteria can cause different kind of infections as opportunistic pathogens, include: 1. ventilator-associated pneumonia ( as one of the common causes) 2. sepsis Sepsis caused by Acinetobacter spp. represents about 2% of total bloodstream infections, and such Infections are mostly correlated with intravascular devices. Meningitis: after neurosurgical procedures Wound infections : in sever trauma and burn wounds UTI : correlated with indwelling urinary catheter 3. 4. 5.
Pathogenicity The pathogenicity of the organism is strongly related to their ability to form biofilm on the surfaces and on human tissues and cells The another important factor is their multidrug-resistance feature ,which make their treatment very difficult. Strains of Acinetobacter that showed resistance to broad-spectrum cephalosporins, -lactam antibiotics, aminoglycosides, quinolones and carbapenems had been reported The bacteria also showed resistance to a wide range of disinfectants, which increase their ability to survive and spread in a hospital setting. The bacteria can also colonize the skin of healthy individual. Health-care associated infection caused by these organisms has become significant global health challenge
Important Virulence factors Capsule : as anti phagocytosis Fimbria : adherence factors to human tissues Pilli: adhesins to environmental surfaces and play a role in biofilm formation MDR encoding gene carried on plasmids and can transmit between strains
Diagnosis Specimens blood sputum pleural fluid Urine Gram stain : gram ve coccobacilli, Culturing : circular, opaque and none mucoid colonies (on nutrient), non lactose fermenter (on MacConkey), and non-hemolysis (on blood agar) Biochemical tests PCR
Treatment Doing antibiotic susceptibility test is crucial to determine which antimicrobial agents is more effective in their treatment In many cases, colistin is the only affective antibiotic. For the more susceptible strains, gentamicin, amikacin, or tobramycin and extended spectrum penicillins or cephalosporins are affective . For the carbapenem resistant strains, tigecycline can be used successfully for treatment. using a combination of antibiotic therapy is necessary for treating the complex infections and multidrug resistant strains
Prevention and control As the bacteria have a strong ability to survive on environmental surfaces for long periods, Some simple measures such as strict hand and environmental hygiene can be applied , which can play a significant role in preventing outbreaks and reducing cross-transmission of infection between health-carers or between patients as well.
References 1. Reidle, S., Morse, S. A., Meitzner, T., and Miller, S. 2019. Jawetz, Melnick & Adelberg s Medical Microbiology , Twenty-Eight Edition. The McGraw-Hill education, Inc. USA 2. Kumar, S. 2012. Textbook of microbiology. Jaypee Brother Medical Publishers (P) Ltd. New Delhi, India 3. Acinetobacter baumannii- Lab Diagnosis, Treatment and Prevention https://microbenotes.com/acinetobacter-baumannii-lab-diagnosis-treatment-and-prevention/ 4. U.S. Center for Disease Control - https://www.cdc.gov/ncidod/dvbid/plague/bacterium.htm