Understanding the Periodontal Ligament in Dental Sciences
The periodontal ligament (PDL) is a vital connective tissue that supports teeth by attaching them to the jaw bone. It consists of various tissues including cementum and alveolar bone, and is rich in vascular and cellular components. The development of PDL fibers plays a crucial role in tooth support and function. Fibers embed in cementum forming Sharpey's fibers and eventually traverse in a coronal direction, forming the intermediate plexus. The structure of PDL includes an hourglass shape with a narrowest point at mid-root level. This ligament's space decreases in non-functional or unerupted teeth.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
PERIODONTAL LIGAMENT DR. K. KISHORE KUMAR, PROFESSOR SIBAR INSTITUTE OF DENTAL SCIENCES DEPARTMENT OF PERIODONTICS
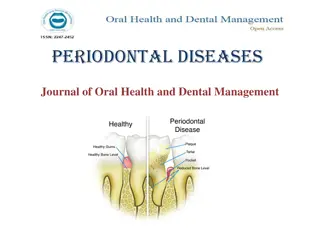
PERIODONTIUM Connective tissue organ that attaches the teeth to the jaw bone & supports during function. Cementum 2 mineralized Alveolar bone Consists of 4 tissues Periodontal ligament 2 soft tissues Lamina propria of gingiva
Periodontal ligament Is a soft, richly vascular & cellular connective tissue that surrounds the roots of the teeth and joins the root cementum with socket wall Extends from base of the socket to apical portion of the lamina propria of gingiva
Development of P.D.L Pdl fibroblasts have their origin in DF &begin to differentiate during root (TENCATE et al 1971) development The outer & inner enamel epithelia fuse & proliferate to form Hertwig's epithelial root sheath
As and when cementum and PDL begin their formation, osteoblasts also differentiate from parafollicular cells and lay down Alveolar bone These fibers embed themselves into the newly formed cementum laid down by cementoblasts at one end, and into the bone laid down by osteoblasts at their other end.
FORMATION OF PERIODONTAL LIGAMENT FIBERS
Initially the fibers become embedded in the cementum as SHARPEYS FIBERS and are laid in coronal direction within the region identified as developing PDL The fibers deposited apical to the CEJ ultimately form the fibers of PDL. By the time approximately 1/3 rd of root formation is complete, fibers are inserted within a cementum matrix from CEJ & traverse in a coronal direction following outline of newly formed crown Both root surface derived & bone derived fibers ultimately coalesce in middle third of ligament to form INTERMEDIATE PLEXUS
Structure of periodontal ligament Average width of periodontal ligament space 0.25 mm (0.2 - 0.4 mm). PDL has a shape of HOURGLASS and is narrowest at mid root level . PDL space diminished around teeth that are not in function & unerupted teeth. PDL has a wavy course when viewed in longitudinal section
Components Fibers Cells Ground substance
FIBROBLAST TROPOCOLLAGEN MOLECULES MICRO FIBRILS FIBRILS FIBER BUNDLE
COLLAGEN It is a protein composed of different aminoacids, most important of them Glycine Proline Hydroxyproline Hydroxylysine Amount of collagen in the tissue can be determined by its hydroxyproline content
Collagen Responsible For Maintenance Of frame work Tone Of Tissue Collagen fibrils have transverse striations with a characteristic periodicity of 64 nm This is due to the overlapping arrangement of tropocollagen molecules
Other than collagen several other proteins also occur proteoglycans glycoproteins (Undulin & fibronectin) Although PDL doesnot contain mature elastin it has two immature forms . oxytalan . Eluanin oxytalan fibers
Oxytalan fibers run parallel to the root surface in vertical direction & they bend attach cementum at cervical third of tooth In addition to these fibers small collagen fibers are associated with larger fibers ,they run in all directions forming INDIFFERENT FIBER PLEXUS
PRINCIPLE FIBRES OF PERIODONTAL LIGAMENT Subdivided into 6 categories 1. Transseptal group 2. Alveolar crest group 3. Horizontal group 4. Oblique group 5. Apical group 6. Interradicular fibers
Transseptal group Extend interproximally over alveolar bone crest and are embedded into adjacent tooth Reconstructed even after destruction Alveolar crest group Arise from crest of alveolar bone & attached to cementum. Resist tilting, extrusive and lateral forces. Horizontal group Alveolar bone to cementum right angles to long axis Resist lateral forces
Oblique group Occupy 2/3rd of the ligament Extend obliquely from cementum to alveolar bone coronally Bear vertical masticatory forces oppose axially directed forces Apical group Fibers radiate in different directions from apex of the tooth Not seen on incompletely formed roots. prevent tooth tipping and extrusion Interradicular group Extend from the crest of the interradicular bone to the furcation area of the multirooted tooth. Fibers are lost if gingival recession extends & the furcation area is exposed.
Cells are divided into 4 main categories: 1. Synthetic cells a. Fibroblasts b. Osteoblasts c. Cementoblasts 2. Resorptive cells a. Osteoclasts b. Fibroblasts c. Cementoclasts 3. Progenitor cells Epithelial rests of Malassez 4. Defense cells a. mast cells b. macrophages
FIBROBLAST Ovoid/elongated, oriented along principal fibers. c/s of fibroblast - stellate appearance Fibroblast are connected by numerous junctions . Gap junction . Adherence type of junction (tight junction) Communication b/n the cells by mutual interaction are facilitated via . Junctional complexus . Electric coupling
GROUND SUBSTANCE The periodontal ligament also contains a large proportion of ground substance filling the spaces between cells and fibers It consists of two main components 1. Glycosaminoglycans - Hyaluronic Acid Proteoglycans 2. Glycoprotein Fibronectin Laminin Also has a high water content(70%)
Functions of PDL Provision of soft tissuecasingto protect the vessels and nerves from injury by mechanical forces 1. 2. Transmission of occlusal forces to bone 3. Attachment of teeth to bone 4. Maintenance of gingival tissues in their proper relationship to teeth 5. Resistance to impact of occlusal forces (shock absorption)
Resistance to impact of occlusal forces (shock absorption) Tensional theory Viscoelastic system theory Tensional theory Principle fiber first unfold ,straighten and then transmit forces to alveolar bone ,causing an elastic deformation of bony socket Finally when bone has reached its limit the load is transmitted to the basal bone
Viscoelastic theory States that displacement of tooth is largely controlled by fluid movements with fibers having only a secondary role When force is transmitted to tooth the extra cellular fluid passes from pdl into marrow spaces of bone through foramina in cribriform plate. The perforations of the plate link the pdl with cancellous portion of alveolar bone and more abundant in cervical third
After depletion of tissue fluids the fiber bundles absorb slack& tighten This leads to blood vessels stenosis Arterial back pressure causes the ballooning of vessels and passage of blood ultra filtrates into tissues and replenish the tissue fluids
Transmission of occlusal forces to bone when an axial force is applied to a tooth a tendency towards displacement of root in to alveolus occurs The oblique fibers alter their wavy, untensed pattern and assume their full length and sustain major part of axial force
When a horizontal work or tipping is applied Two phases of tooth moment occur the first is with in the confines of pdl and Second produces the displacement of the facial and lingual bony plates The tooth rotates about an axis that may change as the force is increased
The apical portion of root moves in a direction opposite to coronal portion In areas of tension the principle fibers are taut rather than wavy In areas of pressure the fibers are compressed, the tooth is displaced Corresponding distortion of bone exists in the direction of root movement
Single rooted tooth-between apical third and middle third Root apex and coronal half of clinical root are other locations of axis of rotation In multirooted tooth axis of rotation is located in bone between the roots Pdl is thinner on mesial surface
Nutritional and sensory functions Pdl supplies nutrients to the cementum ,bone and gingiva by way of blood vessels and also lymphatic drainage pdl is highly vascularized tissue (almost 10% of the volume in rodent molar is blood vessels) This relatively high blood vessel content may provide hydrodynamic damping to applied forces as well as high perfusion rates to pdl
Nerve bundles pass into pdl from the PA area & through channels from the alveolar bone that follow the course of blood vessels The bundles divide into single myelinated fibers which ultimately lose their myelin sheath & end in one of the 4 types of neural termination
1. Free endings tree like configuration carry pain sensation 2. Ruffini like mechano receptors apical area 3. Coiled meissners corpuscles mechano receptors- midroot region 4. Spindle like pressure and vibration endings which are surrounded by fibrous capsule located at apex.
Blood supply Blood vessels 3 sources 1. Vessels that enter the tooth to supply the dental pulp, prior to entry give branches that supply the PDL 2. Intra alveolar vessels traverse horizontally within alveolar bone to enter PDL 3. Gingival vessels supply the P.L from the coronal end
Arterioles and capillaries of microcirculation ramify in Pdl and form a rich network of arcades It is possibly involved that the circulation plays in supporting teeth during function Venous vessels drain axially to drain to the apex
Nerves They are associated with blood vessels and pass through foraminae in the alveolar bone including apical foramen to enter Pdl They run along the length of the root they branch and run coronally & apically Large diameter myelinated Small diameter may or may not be myelinated
Small fibers appear to end in fine branches throughout the ligament Large fibers may end knob like , spindle like , meissner like Large diameter--concerned with pressure Small diameter concerned with pain Lymphatics Lymph vessels provide lymphatic drainage of the P.L. into adjacent alveolar bone
Clinical considerations Pdl thickness varies in different individuals The fact that Pdl is thinnest in middle region of root --- fulcrum of physiologic tooth movement Supporting tissues of tooth long out of function are poorly adapted to carry load suddenly placed on tooth by a restoration
Eg; Teeth opposing bridges or dentures Teeth used as anchorage for removable bridges This will account for inability of a patient to use a restoration immediately after its placement In orthodontic treatment an adjustment period must be permitted
Cysts derived from epithelial cell rests of Malassez Periapical cyst Residual cyst Lateral periodontal cyst Tumours derived from epithelial rests of Malassez Ameloblastoma Primary intra alveolar epidermoid carcinoma Squamous odontogenic tumour