Understanding Bipolar Disorder in Children and Adolescents
Bipolar disorder in young individuals is characterized by mood swings between manic and depressive states, with various subtypes such as Bipolar I, Bipolar II, and Cyclothymia. Clinical characteristics include hypomania and mania, which present with distinct symptoms such as elevated mood, increased activity, and changes in behavior. The disorder typically manifests with symptoms like increased energy, irritability, mood fluctuations, and goal-directed behavior. Recognizing these symptoms early is crucial for appropriate diagnosis and treatment.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
MOOD DISORDERS (BIPOLAR DISORDER, DMDD), AGGRESSION, AND SIB Joshua Proemsey, MD Child and Adolescent Psychiatry Fellow, PGY-5 Division of Child and Adolescent Psychiatry Department of Psychiatry University of Florida
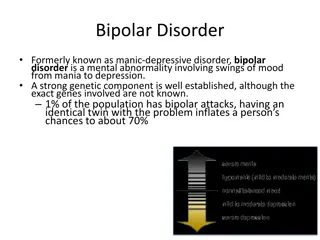
BIPOLAR DISORDER: CLINICAL CHARACTERISTICS Mood disorder characterized by mood swings between manic and depressive states Mood swings are episodic A portion of youth will meet full criteria for Bipolar Disorder although criteria were not designed for Pediatric Populations Normal children will exhibit manic or hypomanic symptoms
BIPOLAR DISORDER: SUBTYPES Bipolar I Disorder: Episodes of mania and depression (14+ days of depression) Mixed episodes can occur Bipolar II Disorder: Episodes of hypomania and depression Cyclothymia: Duration of 1 year with more than half time with episodes of elevated or depressed mood Periods of euthymic mood less than 2 months
BIPOLAR DISORDER: CLINICAL CHARACTERISTICS Hypomania: Mania: Duration: 1 week Duration: 4+ days A) distinct period elevated, expansive or irritable mood A) distinct period elevated, expansive or irritable mood AND persistent increase in goal directed activity or energy B) 3 of following symptoms or 4 of following if mood irritable: AND persistent increase in goal directed activity or energy Inflated self-esteem or grandiosity Decreased need for sleep B) Same as B for mania More talkative than usual or pressure to keep talking C) Unequivocal change from baseline Flight of ideas or racing thoughts D) Noticeable by others Distractibility E) Not severe enough to cause significant impairments, hospitalization and no psychotic features Increase in goal directed activity or psychomotor agitation Excessive involvement in pleasurable activities C) Impairment in functioning or psychosis
BIPOLAR DISORDER: MANIC SYMPTOMS Average age on onset 11.5 years old Most common symptoms; increased energy, irritability, mood lability, distractibility and goal directed activity Least frequent: hypersexuality, hallucinations, delusions Most specific: Grandiosity and Hypersexuality Low specificity: Irritability (common in depression, DMDD, anxiety, PTSD)
BIPOLAR DISORDER: EPIDEMIOLOGY 60% of adults with BP had a mood episode prior to age 20 Prevalence: Pediatric BP-I and BP-II between 1-2% Increased prevalence during late adolescence
BIPOLAR DISORDER: NEUROBIOLOGY Disturbance in Glutamate and GABA in Frontostriatal, Cingulate, DLPFC Neuroimaging: Emotional dysfunction a/w hyper activation of amygdala, PFC, visual Cognitive Deficits related to hypo activation of anterior cingulate cortex Areas of interest: Dysfunction in Emotion Processing (PFC-hippocampal-amygdala circuit) Overactivation of reward processing circuit (left ventral striatal-vlPFC-OFC)
BIPOLAR DISORDER: RISK FACTORS Parents with diagnosed BP Higher rates of bipolar spectrum disorders (23% vs 3%) Higher rates of BP-I (13% vs 1.5%) Offspring with mood lability, subsyndromal manic symptoms and parents with early onset BP approximately 50% risk to develop Genetic Etiology for BP Heritability over 80%
BIPOLAR DISORDER: RISK FACTORS Risk for bipolar in early onset depression is 10-20% Higher risk of conversion to BP in patients with depression when: History of antidepressant-induced or spontaneous hypomania Psychotic features Hypomania Family history of bipolar Psychosocial factors: Low SES, exposure to trauma, stressful family environment
BIPOLAR DISORDER: COMORBIDITIES ADHD - 53% ODD - 42% Conduct Disorder - 27% Anxiety Disorders - 23% Substance Abuse - 9%
BIPOLAR DISORDER: DDX ADHD DMDD ODD / Conduct Unipolar Depression ASD Schizophrenia Substance Use Disorder Borderline Personality Disorder
BIPOLAR DISORDER: DDX Confusion most often ADHD or Behavioral Disorders BP: symptoms of euphoria, grandiosity, decreased need for sleep, hyper sexuality (without h/o abuse), and hallucinations Shared sxs: increased energy, irritability, and aggression More severe in BP youth Other areas: Fhx of Bipolar, response to antidepressants
BIPOLAR DISORDER: DDX ADHD vs Bipolar Recurrent mood swings, outbursts, rages Hallucinations or delusions Later onset of symptoms (10+) FHx of bipolar Symptoms appear abruptly Responded to stimulants and now not responding Symptoms are episodic and a/w mood changes
BIPOLAR DISORDER VS DMDD Behavior problems only occur during an episode of mania or depression Off and on oppositional or conduct symptoms Severe behavioral problems that do not respond to treatment
BIPOLAR DISORDER: TREATMENT OF MANIA / MIXED EPISODES Partial Response to single atypical: First Line: Start with FDA Approved 10-17: Augment with Lithium Abilify, Risperdal, Quetiapine, Asenapine Best data for Risperdal No response: Switch to another FDA approved antipsychotic or Olanzapine Switch to lithium
BIPOLAR DISORDER: DEPRESSION FDA Approved: Latuda and Fluoxetine / Olanzapine combination First, use Latuda If fails, use combination Fluoxetine / Olanzapine If fails, use Lamictal Based upon adult evidence. Evidence sparse in children.
BIPOLAR DISORDER: PSYCHOSOCIAL TREATMENT Psychoeducation: disease management Interpersonal and Social Rhythm Therapy (IPSRT) Cognitive approaches to stress management, emotional regulation and interpersonal conflict Highlights mood regulation causing dysfunction in relationships Discussed regulating sleep and daily rhythms to improve mood regulation and functioning Dialectical Behavioral Therapy (DBT) Focus on emotional regulation and mindfulness
DISRUPTIVE MOOD DYSREGULATION DISORDER Recurrent temper outbursts with negative mood state Diagnostic Criteria: Characterized by frequent, severe, recurrent, temper outbursts and chronically irritable and/or angry mood At least 3 temper outbursts per week Onset aged 6 and no older than 10 years old Must be present for at least 1 year without a symptom free interval of 3 or more months Symptoms presents in 2 of 3 settings: home, social, school
DMDD: COURSE Chronic irritability in early adolescence predicted ADHD in late adolescence and depression in early adulthood Difference between chronic and episodic irritability DMDD increases risk for depression and anxiety in adulthood DMDD does not increase the risk for Bipolar Disorder
DMDD: EPIDEMIOLOGY Lifetime prevalence approx 0.8 - 3.3% Prevalence decreases with age Children with DMDD usually male and younger
DMDD: RISK FACTORS FHx: Stressful events: Substance abuse or Psychopathology Early life trauma Recent h/o divorce, grief Maternal history of peripartum depression Nutritional Iron deficiency, B12 def, Folate def
DMDD: PATHOPHYSIOLOGY Not currently great data specifically on DMDD although data on SMD Hyperarousal elicited by frustrating stimuli During facial affect recognition task, DMDD showed excessive amygdala activation for all faces compared to BP where excessive activation only occurred with fearful faces
DMDD: COMORBIDITIES ODD - 96% ADHD - 81% Anxiety Disorders - 58% Conduct Disorder - 13%
DMDD: NON-PHARMACOLOGICAL TREATMENT Psychotherapeutic Interventions Target impairment in social functioning and emotional dysregulation Behavioral Therapy and Parent Management Training DBT-C - DBT adapted for adolescents include parent training component
DMDD: PHARMACOLOGICAL TREATMENT Evidence limited overall 1st Treat Comorbid Disorders such as ADHD, depression, anxiety if present Antidepressants (SSRI) Useful in treating comorbid anxiety and depression Improved chronic and persistent irritability Remember, DMDD does not have increased rates of bipolar so no increased concern for causing mania Methylphenidate (MPH) Useful for treating comorbid ADHD and improving aggression Optimize medication based upon weight, tolerability and side effects Second Generation Antipsychotics (Abilify / Risperdal) Improved irritability and aggression Concern for side effects
AGGRESSION Aggression and/or irritability is common in many Psychiatric disorders Comprehensive Assessment Modified Overt Aggression Scale (MOAS) - track changes 1st Step - Psychosocial Treatment Parent Management Training (PMT), Parent Child Interaction Training (PCIT), behavioral therapies such as ABA Multimodal interventions such as MultisystemicTherapy Cognitive Behavioral Therapy (CBT) Family Therapy
AGGRESSION: TREATMENT If psychosocial intervention not adequately improve symptoms, consider the following: Treat primary disorder based upon guidelines ADHD, Anxiety, Mood Disorders, etc. Consider Monotherapy with Methylphenidate If fails, consider amphetamine or alpha 2 agonist If fails, then consider Atomoxetine Can combine stimulant with alpha agonist
AGGRESSION: TREATMENT If still struggling, consider using an atypical antipsychotic Low dose Risperdal or Abilify are most frequently used If this fails, consider using the alternative antipsychotic If this fails, consider augmenting with a mood stabilizer
SELF-INJURIOUS BEHAVIOR (SIB) Definition: intentional, self-inflicted damage to the body without suicidal intent Most commonly: cutting, burning, scratching NSSI - nonsuicidal self injurious behavior
SIB: EPIDEMIOLOGY Prevalence approximately 14% in school aged sample in 2002 Not significantly changed since that time Prevalence rates peak around 15-16 yo and decline after 18 Demographics: Adolescence, female
SIB: RISK FACTORS Strongest: former SIB, cluster B traits, hopelessness Strong: previous SI/SA, exposure to peer SIB, abuse Other factors: bullying, negative social interactions, emotional abuse Importance: Significant risk factor for suicide attempts and suicides Significant risk factor for future mental illness even if resolves
SIB: NEUROBIOLOGY SIB frequently related to difficulty with distress tolerance Alterations in Hypothalamic-Pituitary Axis (HPA) Altered Cortisol Response FMRI Differentiated processing of social exclusion Differences in mPFC and vlPFC Patients feel more strongly effected by social exclusion Different activation of limbic system with stress Different activation of opioid system (pain offset) Genetic Factors Altered function of SLC6A4 with polymorphism of 5HTTLPR - increased risk for SIB under stressors
SIB: FUNCTION Automatic Negative Reinforcement (most common reason) Diminishes negative thoughts or feelings Automatic Positive Reinforcement Pleasant thoughts and/or feelings after performing Social Positive Reinforcement (attention, sending message) Social Negative Reinforcement (end argument, get out of activities)
SIB: TREATMENT Medical: wound treatment Psychotherapy: CBT, DBT-A, MBT-A All showed improvement at 12 months ABA or Behavioral Therapy if NDD (Neurodevelopment Disorder) Medications: No medications approved in USA but off-label usage Most commonly use SGAs (Second Generation Antipsychotics) if NDD Risperdal, Abilify Alpha Agonists Clonidine two case reports Opioid antagonists Naltrexone u opioid antagonist blocks release of endogenous endorphins
SIB: TREATMENT PHARMACOTHERAPY N-Acetylcysteine antioxidant and prodrug of cysteine Restores glutathione concentrations in blood and brain Inhibits glutamate release and reduced inflammation Antiepileptics Topiramate believed to reduce through modulation of GABA and glutamate Depakote improves aggression and can improve SIB