Transforming Suicide Assessment, Prevention, and Treatment Approaches
The dedication to those who died feeling unloved and alone is accompanied by a discussion on transforming suicide assessment, prevention, and treatment approaches. The traditional framework and the new consensus in suicide management are explored, emphasizing the importance of involving various stakeholders and targeting suicidality directly. This shift requires increased coordination, focus on the environment of care, and better discharge transitions for individuals at risk.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
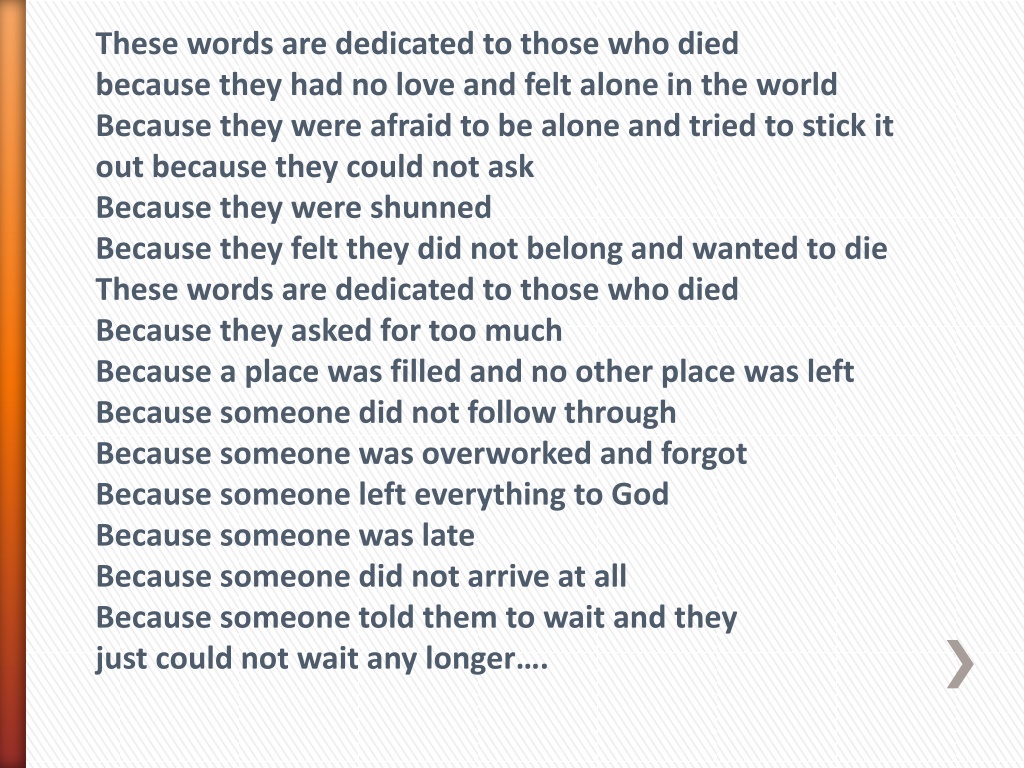
These words are dedicated to those who died because they had no love and felt alone in the world Because they were afraid to be alone and tried to stick it out because they could not ask Because they were shunned Because they felt they did not belong and wanted to die These words are dedicated to those who died Because they asked for too much Because a place was filled and no other place was left Because someone did not follow through Because someone was overworked and forgot Because someone left everything to God Because someone was late Because someone did not arrive at all Because someone told them to wait and they just could not wait any longer .
Transforming Suicide Assessment, Prevention and Treatment Approaches: The New Consensus Susan Stefan
The Traditional Framework A person who threatens suicide is referred to a mental health professional who performs a risk assessment, determines a diagnosis according to presentation, and determines disposition, including voluntary or involuntary inpatient hospitalization, with a focus on keeping the individual safe.
The Traditional Framework: Hospitals 1. ED Assesses People who Arrive with Suicidal Ideation or Attempt for Discharge or Admission 2. If Admitted, Inpatient Unit Provides Safety, Medications, and Groups 3. Contracting for Safety 4. Referral to Outpatient Care on Discharge
The New Consensus **Suicide Researchers **Attempt Survivors/AAS **Joint Commission **CDC **Military **Surgeon General/SAMHSA **Litigation in the Courts
The New Consensus 1. Everyone s Involved 2. Initiate Conversations about Suicide 3. Best Approach: Target Suicidality Directly Rather than as a Symptom of Mental Illness 4. More coordination and followup
The New Consensus: Applied to Hospitals 1. Increased Expectations on ED to both Screen and Assess for Suicidality 2. Increased Focus on Environment of Care 3. Safety plans, NOT contracts for safety 4. Far more coordination with community providers/ensuring appropriate discharge transitions
The New Consensus The New Consensus A. Broadened Participation: We All Need to be Talking More about Suicide 1. PCPs 2. EDs 3. Universities and Colleges 4. Schools 5. Attempt Survivors 6. Friends and Families
Suicidal feelings are not the same as giving up on life. Suicidal feelings often express a powerful and overwhelming need for a different life. Suicidal feelings can mean, in a desperate and unyielding way, a demand for something new. Listen to someone who is suicidal and you often hear a need for change so important, so indispensable, that they would rather die than go on living without the change. And when the person feels powerless to make that change happen, they become suicidal. --Will Hall
Joint Commission Sentinel Alert #56 Places increased responsibility on all health care organizations providing both inpatient and outpatient care esp. primary care providers and emergency departments to better identify and treat individuals with suicidal ideation.
Initiating Dialogue: Screening v. Conversations Despite compelling evidence that screening and risk assessment instruments are not effective, virtually unanimous consensus in favor of screening BUT Attempt survivors want to be listened to, not asked the same predictable questions over and over
When somewhere life breaks the pane of glass, and from every direction casual voices are bringing you the news, you say: I should have known. You say: I should have been aware. I heard rumors of trouble, but after all we all have that. You say: What could I have done? and you go with the rest, to bury him. That night, you turn in your bed to watch the moon rise and somewhere, for someone, life is becoming moment by moment unbearable unbearable Mary Oliver Mary Oliver
Within the narrow methodological limits of the existing literature, existing risk factors are weak and inaccurate predictors of suicidal thoughts and behaviors. Joseph C. Franklin and Jessica D. Ribeiro, Kathryn R. Fox, Kate Bentley, et al. (2017) Risk Factors for Suicidal Thoughts and Behaviors: A Meta- Analysis of 50 Years of Research, Psychology Bulletin 143, 187-232.
C. Suicidality not Mental Illness The Primary Focus of Treatment This is not new: the assessment and treatment of suicidal persons is best conceptualized not in terms of psychiatric categories (such as one finds in the DSM) but rather in terms of psychological pain and the thresholds for enduring that pain. Dr. Edwin Shneidman
What is New: Research Support The extant literature does show that targeting and treating suicidal ideation and behaviors, independent of diagnosis, hold the greatest promise for care of suicidal risk. National Action Alliance for Suicide Prevention (2013)
What is Also New: Suicide-focused Treatment Approaches **CAMS (Joint Commission; NREPP; military; CDC; VA; Menninger Clinic/Houston) **CBT-SP (Joint Commission, NREPP) **DBT (Joint Commission; CDC) **Alternatives to Suicide, Western Mass. RLC, westernmassrlc.org/alternatives-to- suicide
Obstacles to Implementing Treatment Targeted at Suicidality 1. Insurance needs diagnosis for reimbursement. 2. Models are primarily community- based but providers hospitalize rather than learn how to treat suicidal patients in the community, regardless of research findings; hospital stays too short to implement models
No Evidentiary Basis for Inpatient Treatment for Suicidality Hospitalization, by itself, is not a treatment. American Psychiatric Association (2003) Sadly, there is no evidence whatsoever that psychiatric hospitalization prevents suicide American Association of Suicidology/Suicide Prevention Resource Center (2010)
Hospitalization is often necessary for a patient s immediate safety, but hospitalization used solely as a containment strategy may be ineffective or counterproductive and considered by the patient as a disincentive or penalty for expressing suicidal thoughts. Joint Commission (2016)
Whats New for Hospitals Seeing People Who are Suicidal? 1. MORE coordinating with community providers, detailed discharge plans, and followup. 2. Safety plans, NOT contracts for safety 3. Environmental audits 4. Some kind of screening/risk assessment ED and at discharge
DISCHARGE PLANNING *Hospitals own short-term post-discharge suicide risk *Firearm removal *Prescription practices *Telephone followup w/in 24 hours *Community appointment made *Information and education for person and families *Pre-discharge risk assessment
I am myself, even in the dark without mirrors or clues. I may be as inconsequential as the point of a fading penlight but I am not this feeling of being buried alive. If I fall through the ice I am not my hypothermia. I am not my heart's vacuum's cruel absence of presence I am still here