Thymic Neuroendocrine Tumors: Demographics, Treatment, and Survival Study
This study presents an analysis of thymic neuroendocrine tumors (TNET) focusing on demographics, treatment, and survival outcomes. Conducted as a retrospective cohort study using the NCDB data from 2004 to 2015, the study aimed to examine the characteristics of TNET in terms of demographics, clinical features, treatment modalities, and overall survival rates. The research addresses the knowledge gap in understanding the survival outcomes of TNET and sheds light on the diverse aspects of this rare malignancy.
Uploaded on Oct 06, 2024 | 2 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival Charles T. Bakhos MD MS, Aitua Salami MD MPH, Larry Kaiser MD, Roman V. Petrov MD PhD, Abbas E. Abbas MD MS Temple University Hospital, Philadelphia, PA ISMICS Meeting Warsaw, Poland June 2020
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival No disclosures
Introduction Thymic neuroendocrine tumors (TNET): Non-thymomatous malignancy ~ 1 / 5 000 000 US population 1 0.4% of all carcinoid tumors Recently distinguished form thymic carcinomas (WHO) Lack of outcomes data for TNET 1. Chaer R et al. Primary neuroendocrine tumors of the thymus. Ann Thorac Surg 2002
Introduction Knowledge gap: Survival outcomes of TNET have not been thoroughly compared Study aim: To examine the demographic, clinical, treatment and survival characteristics of TNET.
Methods Study design: Retrospective cohort study using the NCDB (2004 2015) Inclusion criteria: Histologic diagnosis of TNET WHO ICD-0-3 Exclusion criteria: Age < 18 years Incomplete staging data
Methods Primary outcomes: Overall survival Secondary outcomes: Demographic, clinical, treatment characteristics Statistical analyses: Survival analyses Multivariable logistic and cox regression
Demographic and Clinical Characteristics TNET Variables N = 295 (%) 57 (24) 208 (70.5) 233 (79.0) 278 (94) 226 (76.6) 7.3 (6.0) Age in years, Median (IQR) Male Caucasian Insured Charlson-Deyo score (0) Median tumor size (cm), (IQR) Tumor stage Localized Regional Distant Median follow up in years, (IQR) 134 (45.4) 140 (47.5) 21 (7.1) 3.8 (4.5)
Distribution of TNET (N = 295) 48.5% 32.2% 10.5% 8.8% Typical Carcinoid Atypical Carcinoid Small Cell Large Cell
Treatment Characteristics TNET Variables N = 295 (%) Treatment received Chemotherapy Radiation therapy Chemoradiation Surgery Trimodality therapy 103 (34.9) 116 (39.3) 30 (10.2) 172 (58.3) 34 (11.5)
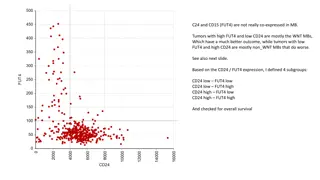
Treatment Characteristics Variable Age in years Hazard Ratio 1.02 Confidence Interval 1.010 1.038 p-value 0.001 Variable Hazard Ratio Ref Confidence Interval p-value Tumor Stage (Localized) Age in years 1.02 1.010 1.038 0.001 Tumor Stage (Localized) Regional 1.54 1.04 2.30 0.031 Ref Regional Distant 1.54 2.65 1.04 2.30 0.031 1.31 5.35 0.006 Distant 2.65 3.54 1.31 5.35 0.006 Chemotherapy only 2.05 6.12 <0.001 Chemotherapy only 3.54 2.05 6.12 <0.001 Trimodality therapy 0.33 0.33 0.14 0.75 0.008 Trimodality therapy 0.14 0.75 0.008
Survival Outcomes Following Radiation for TNET with Positive Resection Margins
Treatment Characteristics Variables Hazard Ratio Confidence Interval P Chemotherapy None Neoadjuvant chemotherapy Adjuvant chemotherapy Radiation therapy None Adjuvant radiation therapy Age in years Tumor stage Localized Regional Distant Positive resection margin Ref 0.36 1.09 0.17 0.74 0.73 1.63 0.006 0.669 Ref 0.36 1.02 0.25 0.53 1.01 1.03 <0.001 <0.001 Ref 4.24 8.98 2.24 2.92 6.14 5.34 15.09 1.62 3.11 <0.001 <0.001 <0.001
Limitations Retrospective study design Selection bias Residual confounding Administrative dataset No data on baseline functional status, postoperative complications, tumor recurrence Staging system Lack of lymph node sampling
Conclusions TNET are rare and aggressive mediastinal tumors of the thymus Trimodality therapy is associated with improved survival Lymph node dissection seems to be underutilized in the surgical treatment of TNET. Adjuvant radiation is associated with improved survival for margin positive TNET. Prospective studies are warranted to better clarify the treatment algorithm for TNET.
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival Charles T. Bakhos MD MS, Aitua Salami MD, Larry Kaiser MD, Roman V. Petrov MD PhD, Abbas E. Abbas MD MS