The New Pain Complications of Mesh Inguinal Hernia
Understand the complications, definitions, incidence, natural history, symptoms, and diagnosis of chronic post-surgical pain associated with mesh inguinal hernia. Explore insights from Professor Michael O'Rourke and other experts.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
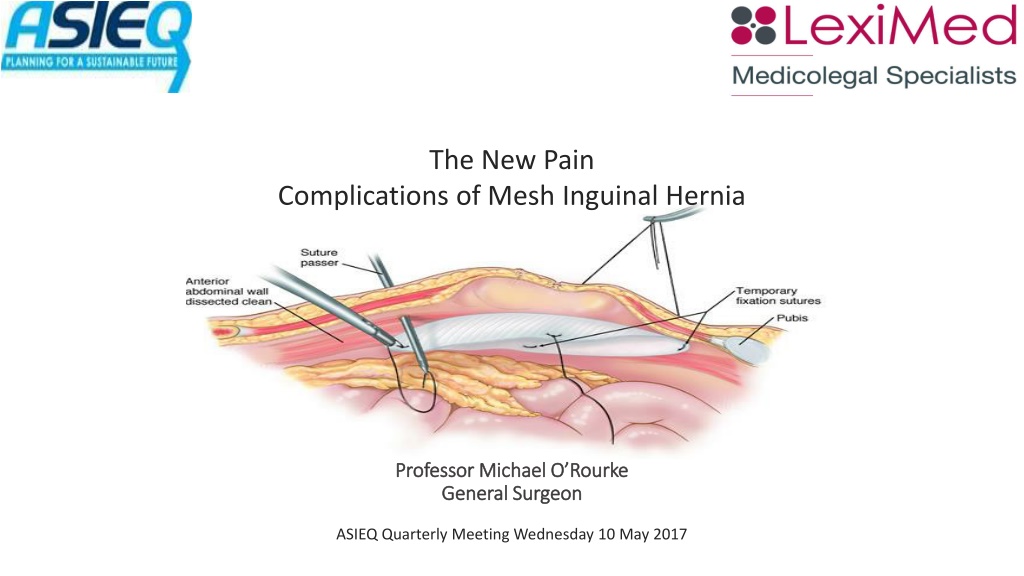
The New Pain Complications of Mesh Inguinal Hernia Professor Michael O Rourke Professor Michael O Rourke General Surgeon General Surgeon ASIEQ Quarterly Meeting Wednesday 10 May 2017
Complications Complications 1. Post Hernia Repair Pain or CPSP. 2. Recurrence. 3. Wound Infections.
Definitions Definitions CPSP: Chronic post surgical pain. Pain that has been present continuously for longer than 3 months. And longer than 6 months. Reference: 1986 International Assoc for Pain Study, 2011 Alfieri et alia.
Incidence (1) Incidence (1) Pain has supplemented recurrence as a complication of surgery. The increased incidence of pain mirrors a parallel increase in the use of polythene meshes. Reference: Bendavid et alia Hernia 2015
Incidence (2) Incidence (2) 1. O Rourke & O Rourke 6-54% - (6 Studies) ANZ J .of. S 2012. 2. Langeveld Rotterdam 27% - Hernia 2015. 3. Westin et alia Laparoscopic 20% Open 33% Annals of Surg 2016.
Natural History (1) Natural History (1) Most pain resolves in the first 12 months, generally CPSP is treatment resistant, it eventually dissipates with time, it is impossible to prognosticate when. Reference: Sanblom (K) J.Pain Res 2015 Geticis J.Am Coll Surg 2015
Natural History (2) Natural History (2) 1. Neuropathic pain or 2. Nociceptive pain or pain due to tissue injury or inflammation.
Symptoms CPSP Symptoms CPSP May be burning, tingling or electric shock like pain, may be associated with paraesthesia, anaesthesia, hyperaesthesia or allodynia. This is more typical of neuropathic pain. Pain due to other pathology or nociceptive pain is usually less severe. V.V difficult to differentiate. Reference: Voorbrood Hernia 2015
Diagnosis CPSP Diagnosis CPSP 1. Exclude other pathology e.g. hip, back, adductor muscles. 2. MRI / CT is of little value in diagnosis of CPSP. 3. History probably best for differentiating neuropathic from other pathology but it is unreliable. 4. Use of algorithm e.g. history, physical signs, past and family history, psychiatric history, previous environments e.g. work and insurance status. Reference: Voorbrood Hernia 2015
Treatment Treatment 1. Prevention. 2. Neuropathic pain refer to a pain clinic for at least 12 months. 3. Treatment of non-neuropathic pathology. 4. Wait for late resolution. 5. Surgery for persistent pain!!
Prevention Prevention Instead of mesh therapy being the sole surgical technique: A. With young males and females with indirect Hernia excise the sac and tissue repair. B. Patients with severe pain and a reducible lump allow the pain to settle pre-op +/- temporary truss. C. No lump no hernia groin pain and ultrasound diagnosis of hernia is no indication for surgery. It is the duty of every surgeon to avoid iatrogenic complications.
Rationale for repeat surgery Rationale for repeat surgery 1. Triple neurectomy. 2. Mesh removal, re-innervation or neo innervation. 3. Treatment of recurrence. Many patients want surgery think something went wrong.
Triple Triple Neurectomy Neurectomy 1. Wantz no nerve no pain. 2. Prospective randomized trials no benefit dividing nor preserving the 3 nerves. 3. Post-mesh implant Marked fibrosis and difficulty finding 3 nerves. 4. Invalid claims by a few. Reference: Amid Hernia 2011
Surgical Reports Surgical Reports 1. Sun et Alia Mayo clinic 43% >12 months Multiple procedures Am J. of Surg 2016 2. Calleson et Alia Hernia recurrence and pain High post op neuropathic pain B.J of Surg 1999 3. Valvekens One In three pain free Hernia 2015 4. Amid 90% Cure with triple neurectomy
Surgical Negligence Surgical Negligence 1. Yes it is an iatrogenic complication. 2. Excuses: All from correspondence a) Not due to surgery. b) Never had this before. c) Just take analgesics and it will go away. d) Referred back to General Practitioner to cope. e) Referred to sports medicine doctor. f) Need to re-explore.
Summary Summary 1. CPSP is iatrogenic. 2. The incidence is high 20-30%. 3. There is a high incidence of spontaneous resolution. 4. Treatment is difficult. 5. The role of interventional procedures is still unknown.
GEPI GEPI The Queensland Workers Compensation Scheme Guidelines for Evaluation of Permanent Impairment, 2nd Edition, Chapter 16, Page 94. 16.2 AMA5, p 136: section 6.6 hernias. Occasionally in regard to inguinal hernias there is damage to the ilio-inguinal nerve following surgical repair. Where there is loss of sensation in the distribution of the ilio- inguinal nerve involving the upper anterior medial aspect of the thigh, a one percent Whole Person Impairment should be assessed as per Table 5.1 of this Guide. This assessment should not be made unless the symptoms have persisted for twelve months.
AMA5 AMA5 The American Medical Association s Guides to the Evaluation of Permanent Impairment, 5th Edition, Chapter 6, Page 136. Table 6-9 Criteria for Rating Permanent Impairment Due to Herniation Class 1 0% - 9% Impairment of the Whole Person Class 2 10% - 19% Impairment of the Whole Person Class 3 20% - 30% Impairment of the Whole Person Palpable defect in supporting structures of abdominal wall and Slight protrusion at site of defect with increased abdominal pressure, readily reducible or Occasional mild discomfort at site of defect but not precluding most activities of daily living. Palpable defect in supporting structures of abdominal wall and Frequent or persistent protrusion at site of defect with increased abdominal pressure, manually reducible or Frequent discomfort, precluding heavy lifting but not hampering some activities of daily living. Palpable defect in supporting structures of abdominal wall and Persistent, irreducible, or irreparable protrusion at site of defect and Limitation in activities of daily living.
Professor Michael G.E. ORourke AM.M.B., B.S., F.R.C.S., F.R.C.S.Ed., F.R.A.C.S., F.A.C.S. F.Q.I.M.R. General Surgeon