Risk Reduction in Cardiovascular Patients: Beyond Lipids
In this presentation, Dr. Jenny Rajala delves into strategies for reducing cardiovascular risk beyond lipid management. The slides discuss various aspects including financial disclosures, conflict of interest mitigation, patient case studies, and the role of aspirin in primary prevention. Detailed insights on primary prevention efficacy and risk factors are provided based on meta-analyses and randomized trials.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Risk Reduction in the Cardiovascular Patient: Outside of Lipids Dine and Learn Nov 30, 2022 Dr. Jenny Rajala
CFPC CoI Templates: Slide 1 used in Faculty presentation only. Faculty/Presenter Disclosure Faculty: Dr. Jennifer Rajala Relationships with financial sponsors: Any direct financial relationships including receipt of honoraria: Pfizer, Bayer, Boehringer- Ingelheim, CardioMetabolic Collaborative Clinic Memberships on advisory boards or speakers bureau: Nil Patents for drugs or devices: Nil Other: financial relationships/investments Nil
CFPC CoI Templates: Slide 2 Disclosure of Financial Support This program has received financial support from the South Island Division of Family Practice in the form of an educational grant Potential for conflict(s) of interest: Dr. Jennifer Rajala has received payment from Doctors of BC for this session AND previously received payments from Bayer for prior talks about medications that will be discussed tonight.
CFPC CoI Templates: Slide 3 Mitigating Potential Bias The talk involves generic medications wherever possible Use of randomized trials and meta-analysis where possible to guide decisions Use of guidelines where appropriate
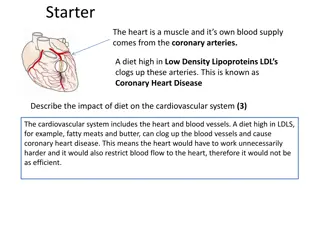
Kathy 72F Prior multivessel PCI for 3 separate NSTEMIs over the past 8 years Carotid endarterectomy 5 years ago 2 block claudication HTN Type 2 diabetes mellitus, HbA1c 7.8% Dyslipidemia, non-HDL controlled at 2.1 Ex-smoker, quit 8 years ago Medications: Aspirin 81 mg daily Ramipril 5 mg BID Bisoprolol 2.5 mg daily Chlorthalidone 25 mg daily Atorvastatin 80 mg daily Metformin 850 mg TID Gliclazide 60 mg daily On examination: 115/76, HR 65 bpm Normal cardiac exam Femoral bruits present
Aspirin Primary prevention Secondary prevention Long term DAPT Peri-operative management
Primary prevention In meta-analysis of 10 RCTs of primary prevention the use of low dose ASA was associated with: MACE RR 0.89 (95% CI 0.84-0.93) MI RR 0.86 (95% CI 0.78-0.95) Ischemic stroke RR 0.84 (95% CI 0.76-0.93) Major bleeding RR 1.42 (95% CI 1.26-1.60) Intracranial hemorrhage RR 1.33 (95% CI 1.11-1.59) GI bleeding RR 1.91 (95% CI 1.44-2.54) NNT for MACE: high risk 682, low risk 2191 NNH major bleeding: high risk 983, low risk 819 American Journal of Cardiovascular Drugs 2022; 22:657
Secondary Prevention Figure 3 Lancet 2009;373(9678):1849
Long term DAPT DAPT trial 9961 pts with DES randomized to plavix or prasugrel and ASA vs ASA alone during the period of 12-30 months post PCI Stent thrombosis 0.4% in DAPT vs 1.4% SAPT (p<0.001) MACE 4.3% DAPT vs 5.9% SAPT (p<0.001) All cause death 2.0% DAPT vs 1.5% SAPT (p = 0.05) Moderate or severe bleeding 2.5% DAPT vs 1.6% SAPT (p=0.001) Pegasus- TIMI 54 trial 21162 patients with MI to 1-3 years of ASA with ticagrelor 90 mg BID, 60 mg BID or placebo CV death, MI, or CVA in 7.85% tica 90 BID, 7.77% tica 60 BID, and 9.04% placebo (p = 0.004 for 90 BID dose and 0.008 for 60 BID dose vs placebo) TIMI major bleeding 2.60% with 90 BID, 2.30% with 60 BID, and 1.06% with placebo (p <0.001 for each dose vs placebo) 1. NEJM 2014; 371:2155 2. NEJM 2015; 372:1791
Long Term DAPT Consider for patients who have a low bleeding risk and tolerate DAPT for 1 year who have high risk clinical features for thrombotic events CCS 2018 Antiplatelet Guidelines
Guidelines Use of SGLT2i and GLP-1 RA have been incorporated into both American Diabetes Association and ESC 2019 Guidelines on Diabetes, Pre-Diabetes and CardioVascular disease 2022 Canadian Cardiovascular Society Guideline for Use of GLP-1 Receptor Antagonists and SGLT2 Inhibitors for Cardiorenal Risk Reduction Can J Cardiol 2022;38(8):1153
Dual Pathway Inhibition with Rivaroxaban Vascular Dose 2.5 mg bid + ASA Reduced CV Death, Stroke and MI 10 ASA 100mg od Rivaroxaban 5mg bid 5.4% Rivaroxaban 2.5mg bid + ASA 100mg od 8 4.9% Cumulative incidence (%) 4.1% ARR for ASA vs Riva 2.5 BID + ASA = 1.3% NNT = 77 6 4 MACE* % HR (95% CI) p-value 2 ASA 100mg OD 5.4 - - Rivaroxaban 5mg BID 4.9 0.90 (0.79-1.03) 0.12 Rivaroxaban 2.5mg BID + ASA 100 mg OD 4.1 0.76 (0.66-0.86) <0.001 0 0 1 2 3 Year Number at risk ASA 100mg od Riva 5mg bid Riva 2.5mg bid + ASA 100mg od 9126 9117 7808 7824 3860 3862 669 670 9152 7904 3912 658 *Rates as at mean follow up of 23 months Eikelboom JW et al. N Engl J Med 2017; 377:1319-30
Consistent Benefit of Dual Pathway Inhibition with Rivaroxaban Vascular Dose 2.5 mg bid + ASA in CAD Patients with PAD Rivaroxaban 2.5 mg bid + ASA n/N (%) p-value (intx) ASA alone n/N (%) ARR/ ARI Subgroup HR (95% CI) HR (95% CI) CV Death, Stroke or MI Peripheral artery disease Yes No NNT= 37 0.37 ARR 2.73 1.06 94/1656 253/6657 (5.7) (4) 138/1641 322/6620 (8.4) (5) 0.67 (0.52-0.87) 0.77 (0.66-0.91) Major Bleeding Peripheral artery disease Yes No NNH= 106 0.46 ARI 0.95 1.33 52/1656 211/6657 (3) (3) 36/1641 122/6620 (2) (2) 1.43 (0.93-2.19) 1.73 (1.38-2.16) Net Clinical Benefit Peripheral artery disease Yes No NNT= 37 0.24 101/1656 291/6657 (6) (4) 145/1641 349/6620 (9) (5) 0.68 (0.53-0.88) 0.82 (0.71-0.96) 0.1 1 10 Favours ASA alone Favours rivaroxaban 2.5 mg bid + ASA Connolly SJ et al. Lancet 2018;391:205 218.
CCS 2022 Guidelines on Peripheral Arterial Disease