Prescription Drug Pricing
Virginia Government Relations Director at American Cancer Society Cancer Action Network focuses on solutions to make prescription drugs more affordable for patients, addressing high out-of-pocket costs and advocating for legislative reforms to improve access to medications and reduce financial burden on individuals with chronic conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Prescription Drug Pricing Solutions to Lower Costs for Patients Brian Donohue Virginia Government Relations Director American Cancer Society Cancer Action Network
ACS CAN The American Cancer Society Cancer Action Network (ACS CAN) is making access to care, health equity, and affordability for cancer patients a top priority for public officials and candidates at the federal, state and local levels. ACS CAN empowers advocates across the country to make their voices heard and influence evidence-based public policy change as well as legislative and regulatory solutions that will reduce the cancer burden. As the American Cancer Society s nonprofit, nonpartisan advocacy affiliate, ACS CAN is critical to the fight for a world without cancer. www.fightcancer.org.
Patients Should Come First American Cancer Society Cancer Action Network is dedicated to improving access to quality, affordable, and equitable healthcare in Virginia. Access to prescription drugs often comes down to co-pays or cost sharing. We are interested in solutions that will make prescription drugs affordable to the patient. These solutions must not only include pharmaceutical manufacturers but encompass all health care stakeholders, including insurance companies, wholesalers, pharmacy benefit managers, and others who restrict access to care and continuously shift costs onto patients. Patients out-of-pocket costs for prescription drugs in the form of high deductibles and co-insurance have continued to create critical access and affordability challenges for those with chronic conditions. Repeated studies have verified that high OOP costs are a significant barrier to treatment and often lead to skipped doses or outright abandonment of treatment.
Thank You Patient Access Wins in Virginia In 2019, Virginia was the first state to pass HB2515 Accumulator Adjustment ban, legislation ensuring that co-pay assistance programs (coupons) count toward patient s deductible and out-of-pocket maximums. This year the step therapy reform law went into effect which increases access to needed medications for patients that physicians feel are appropriate. HB 66 was signed into law by Governor Northam this session which caps patient s out of pocket costs for prescription insulin to a maximum of $50 a month for a 30-day supply.
Directly Address Patient Out-of-Pocket Costs Cap patient s out of pocket costs for prescriptions. Virginia legislators should consider expanding HB 66 (Insulin Cap) to include all prescription medications to decrease prescription costs for patients. Similar bills have passed in DC and Maryland that limit a patient s out of pocket costs to a maximum of $150 per month for specialty medications. Promote predictability by ensuring patients have access to plans with fixed copays across all prescription drug tiers rather than using high co-insurance levels. Increase choice in the insurance marketplace by ensuring that some plans offer benefit designs with no prescription drug deductible. Ensure non-discrimination by prohibiting plan designs that discriminate against individuals based on health status or claims experience and place all medicines used to treat a condition on the highest cost-sharing tier.
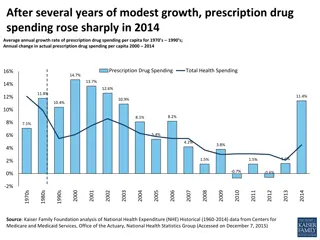
Eliminate Drug Rebates or Pass the Savings to Patients Virginia should consider making sure rebates and discounts are shared with patients at the pharmacy. On average, pharmaceutical companies rebate about 40 percent of a medicine s list price back to health insurance companies and pharmacy benefit managers. Currently, these rebates and discounts are not reaching patients at the pharmacy counter. They stay with the health insurers and pharmacy benefit managers. These rebates and discounts should be shared with patients at the pharmacy counter or used to lower patient premiums.
Increase Accessibility of Biosimilars Biosimilars are biologic medicines approved by the FDA as highly similar to the original biologic medicine that work in the same way and have no clinically meaningful difference in safety or efficacy. Biosimilars have been approved for a wide range of conditions, including autoimmune diseases such as rheumatoid and psoriatic arthritis, and certain types of cancers. Like generics for traditional medicines, biosimilars may offer lower-cost choices for patients who take biologic medicines. Formulary restrictions and the current rebate structure continue to be barriers. Improved access for biologics should translate into more affordable out-of-pocket costs for patients.
State Legislation - Best Practices Formulary transparency Help consumers shop for prescription drug coverage Clear information about what drugs are covered and what out-of-pocket costs will be in a dollar amount Banning mid-year switching Ensure that the drug coverage that was disclosed to the consumer at open enrollment remains in effect throughout the plan year No changes to drugs covered No changes to out-of-pocket costs
State Legislation - Best Practices Prior authorization Streamline this process Insurers and doctors use one standard form Insurers must respond to requests within certain timeframes Step therapy Identify when patients should be exempt from a step therapy protocol Allow doctors to request an exception Insurers must respond to requests within certain timeframes
State Legislation - Best Practices Copay-only health plans Limit the use of coinsurance in prescription drug coverage Coinsurance is often an unknown amount = percentage of a drug s price Require one-quarter of plans offered to have copayments only (fixed dollar amount per drug) Medication synchronization Patients with multiple prescriptions can synchronize their refill date Often allows for partial, pro-rated copayments Limits trips to the pharmacy