Pediatric CRRT Prescription: Rates, Dose, Fluids Overview
This informative content by Dr. Michael Zappitelli from Montreal Children's Hospital discusses the prescription rates, doses, and fluids involved in Pediatric CRRT. It covers insights on blood flow rates, diverse solutions used, and ideal compositions for Peritoneal dialysis fluid. The article emphasizes adjusting blood flow rates based on age and weight, promoting circuit lifespan, and monitoring for clot formations. Additionally, the importance of replacing fluids to achieve solute clearance by convection in CVVH treatment is highlighted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
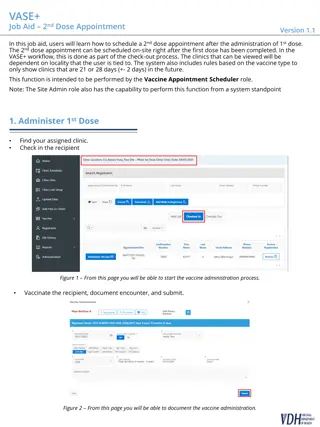
PEDIATRIC CRRT THE PRESCRIPTION: RATES, DOSE, FLUIDS Michael Zappitelli, MD, MSc Montreal Children's Hospital McGill University Health Centre
OVERVIEW Rates & Dose Blood flow Dialysis fluid Suggested Replacement fluid Not necessarily a recipe Ultrafiltration rate Fluids
BLOOD FLOW RATE Qb Age & weight based Promote circuit lifespan + patient stability: clots vs alarms Highly access-dependent Aim return access pressures ~ < 200 mmHg, no alarms May be machine dependent Prisma: 180 ml/min Prismaflex & Aquarius: 450 ml/min Start lower and increase by about 10 minutes (?)
BLOOD FLOW RATE No set perfect rates From 3 to ~10 ml/kg/min, depending on age: Examples: 0-10 kg: 11-20kg: 21-50kg: >50kg: 25-50ml/min 80-100ml/min 100-150ml/min 150-180ml/min Based on previously most commonly used machine Neonates 8 to 12 ml/kg/min Children 4 to 8 ml/kg/min Older 2 to 4 ml/kg/min. Most not > 200 ml/min: not dangerous just not necessary
BLOOD FLOW RATE May need to modify: Be aware of access and return pressure Visually inspect filter for clots Transmembrane pressure may need to increase blood flow Filtration fraction
SOLUTIONS Slow continuous ultrafiltration none CCVHD dialysis fluid for diffusive clearance CVVH replacement fluid: replacing fluid you are removing to achieve solute clearance by convection CVVHDF both Using these to correct metabolic abnormalities (remove) and prevent treatment-related metabolic abnormalities (replace).
IDEAL SOLUTIONS Peritoneal dialysis fluid? Hyperglycemia, metab acidosis Soysal et al, Ped Neph, 2007 Physiological/ compatible Composition: Sodium: ~ 130 to 140 Chloride: ~105 to 120 dependent on other anions (HCO3) Potassium: MOST Zero need to add (some have) Magnesium: 1 to 1.5 mEq/L Glucose/Dextrose: 0 to 110 mg/dL Lactate: Most 0 to 3 mEq/L (35-40 mEq/L if lactate buffer) Bicarbonate: Reliable Pre-made IV solutions: Saline, Lactated Ringers Inexpensive Easy to prepare Multi-bag systems: why? Custom-made solutions: Local pharmacy; outsource Most 30-35 mEq/L Few ZERO As low as 22 to 25 mEq/L Simple to store Quick to the bedside Commercially available solutions: Ready-bags (compartments) Concentrate added to bag Widely available Calcium: 0 to 3.5 mEq/L
CHOOSING SOLUTIONS Cost (Storing, frequency of use) Anticoagulation: +/- calcium with citrate anticoagulation There are citrate based solutions and data Patient safety patient volume? Does everyone prescribing really understand? Regulatory issues (dialysis versus replacement fluid....) Accusol Normocarb Duosol Prismasate Some solutions are more flexible than others Prismasol Hemosol BO ...........
PHOSPHATE They WILL develop hypophosphatemia Can replace: IV boluses, TPN MANY add it to solutions but no good data Worry about precipitation, calcium-magnesium binding How much too much? No good answer. Many 1.2-1.5 mmol/L Pharmacy versus nurse-based addition?
ADDING PHOSPHATE et al, Intens Intens Care Med, 2004 Care Med, 2004 Experiment Experiment Added 1.2 mmol/L PO4- to calcium rich solutions 5 hours: no effect on calcium, bicarb, pH, pCO2 No visual precipitation With and without filtering 2 days: to precipitation bags will not need to be hung for more than a day Troyanov Troyanov et al, Santiago et al, Santiago et al, Therap Consideration: Consideration: Therap Apher Experiment Experiment Apher & Dialysis, 2010 & Dialysis, 2010 Added NaPO4 to dialysis/replacement fluid bags (12) containing calcium and magnesium 0.8 mmol/L 1.5 mmol/L 2.5 mmol/L Experiment Experiment Pre-post evaluation of adding NaPO4 to dial & replace solution Most dialysis or replacement fluid Retrospective clinical Retrospective clinical 14 adults CVVHDF KPO4 added when <1.5 mmol/L (protocolized) No negative effects caused on calcium, bicarb, pH 0.8 mmol/L, 47 children, solutions contained Ca++ & Mg++ Santiago et al, KI, 2009 Santiago et al, KI, 2009 No change in calcium, magnesium, sodium, gluc, pH 2, 24 and 48 hours No precipitation seen Less IV PO4 needed
DIALYSIS FLUID? REPLACEMENT FLUID? Personal suggestion: use the same solution If needed (e.g. alkalosis) can modify the replacement solution Regulatory issues may hinder: Replacement solution saline, with additives
ALBUMIN DIALYSIS Removes protein bound small substances: e.g. copper/Wilson's, drugs, toxins of liver failure Albumin live a scavenger Dialysis: albumin-containing solution across highly permeable membrane 25% albumin added to dialysis fluid bag: 2-5% albumin solution it's single pass - bags are changed Shouldn't affect sodium may affect (reduce) other electrolytes Theoretically may affect citrate anticoagg rates Allergic reaction Collins et al, Pediatr Nephrol, 2008 Askenazi et al, Pediatrics, 2004 Ringe, Pediatr Crit Care Med, 2011
SOLUTIONS: WATCH FOR ERRORS! Barletta et al, Pediatr Nephrol, 2006 Soysal et al, Pediatr Nephrol, 2007 Survey: ICU, Nephrology, CRRT 16/31 programs reported solution compounding errors 2 deaths 1 non lethal cardiac arrest 6 seizures (hypo/hypernatremia) 7 without complications Country where resources dictate need to use PD solution for dialysis and NS + additives for replacement fluid Many reported electrolyte complications: glucose, sodium, acidosis
DIALYSIS AND REPLACEMENT FLUID RATES: CLEARANCE & DOSE Clearance mostly a function of: Dialysis fluid flow rate (Qd) Replacement fluid flow rate (Qr) Qd + Qr (CVVHDF) Higher rates = higher clearance for IEM, drug removal, severe high K = more middle molecule clearance (CVVH/CVVHDF) = more hypophosphatemia, kalemia, magnesemia = more amino acid losses = more drug clearance = more CITRATE clearance = more work to change bags, give electrolyte infusions Lower rates simplify electrolyte balance and limit protein loss
DIALYSIS AND REPLACEMENT FLUID RATES: CLEARANCE & DOSE No well-defined right dose of clearance. For CRRT:mostly expressed in terms of effluent(ml/kg) per hour Standard suggestion: Urea clearance ~ 30-40 ml/min/1.73msq Qd or Qr or Qd+Qr ~ 20-40 ml/kg/hour OR 2 to 2.5 liters/hr/1.73msq. Some do much higher: some machines as high as 8L/hour REALIZE: What you prescribe is not necessarily what the patient gets!! Time off circuit, microclots in filter over time, predilution
10 KG CHILD: 30 ML/KG/HR CLEARANCE OR ~ 0.26 MSQ: 2L/1.73MSQ/HOUR = 300 ML/HOUR CVVH Qr = 300 ml/hour CVVHDF CVVHDF Qd = 150ml/hour Qr = 150 ml/hour CVVHD Qd = 300 ml/hour
ULTRAFILTRATION/FLUID REMOVAL RATES No Study has identified effective, safe UF rates in Children. General acceptance that 1-2ml/kg/hr is often safe (stable patient) Choose UF rate to: balance input (e.g. boluses, citrate, calcium, etc) remove excess fluid over time make room for IV fluids and nutrition Also provides solute clearance by convection
ULTRAFILTRATION/FLUID REMOVAL RATES Fluid removal should be safe AND effective no need to sacrifice one for other: Frequent communication Frequent reassessment (MD), Hourly reassessment (RN) Know what the usual hourly input is : IV fluids Citrate & calcium Nutrition (give!!) Meds/infusions Provide rules for removing intermittent fluids Be aware of the outs (tubes, urine, diarrhea) account for
ULTRAFILTRATION/FLUID REMOVAL RATES Decide desired DAILY fluid removal, after understanding TOTAL severity of Fluid Overload Assure safety of this desired daily fluid removal Decide desired hourly negative balance Even balance?: Simply remove hourly ins significant outs Negative balance?: Same + remove desired negative balance Think about filtration fraction make sure not too high UFR/Plasma flow rate --- UFR/Qb <20-25% CVVHD or post-filter CVVH <30-35% pre-filter CVVH
SUMMARY Blood flow: balance access/circuit life with tolerability Solutions: Many choices Know their content, regional rules, CRRT type used Decide on desired flexibility Decide what's best for your institution (volume, expertise) Bicarbonate and calcium are most substantial differences Be aware of errors Dialysis/replacement fluid rates: ie clearance dose Balance desired clearance with undesired losses 2-2.5 L/hour/1.73msq suggested only Ultrafiltration rate: Frequent reassessment, team team + targeted Safety AND efficacy are feasible targeted fluid removal decisions