Outcomes of Parastomal Hernia Repair in Inflammatory Bowel Disease Patients
This study examines the outcomes of parastomal hernia repair in patients with inflammatory bowel disease, specifically comparing outcomes between those with Crohn's disease and ulcerative colitis. The research, conducted from 2012 to 2022, analyzes data from 392 patients, highlighting factors such as follow-up duration, demographics, comorbidities, and operative details. Findings reveal significant differences between the two patient groups, emphasizing the complexity of managing parastomal hernias in individuals with IBD.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Parastomal Hernia Repair Outcomes in Patients with Inflammatory Bowel Disease Lucas Beffa, MD, FACS Assistant Professor of Surgery Lerner College of Medicine Cleveland Clinic Co-authors: Ben Miller, MD; Sara Maskal, MD; Ryan Ellis, MD Mike Rosen, MD; Clayton Petro, MD; Sharon Phillips, PhD; David Krpata, MD; Ajita Prabhu, MD
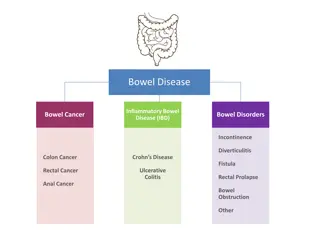
Parastomal Hernias Parastomal hernias alone are challenging to repair with high rates of complications IBD patients represent a unique population given their multiple surgeries, and high likelihood of requiring future operations
Aim To describe the outcomes of parastomal hernia repair in patients with inflammatory bowel disease and compare those outcomes in patients with CD to UC
Methods ACHQC search from 2012 -2022 for patients with IBD and Parastomal hernia repairs with at least 30 day follow up
Results 392 patients met criteria - 182 CD - 210 UC
Follow Up Breakdown CD (182) UC (210) Total (392) 30 day follow up 182 210 392 30 day - 1 year follow up 57 114 171 1 - 4 year follow up 85 170 255
Ulcerative Colitis (N=210) p-value Crohn s disease (N=182) 57% (104) 40% (85) < 0.001 Female 0.008 Race White Non-white 91.7% (165) 8.3% (15) 97.6% (204) 2.4% (5) 54 (44,63) 63 (53,71) <0.001 Age, median (IQR) 0.001 Smoking status Current Former Distant Never 9.0% ( 16) 5.7% ( 10) 20.3% (36) 65.0% (115) 2.0% (4) 1.5% (3) 19.7% (40) 76.8% (156) 31 (27,35) 32 (28, 36) 0.16 BMI, median (IQR) Comorbidities Hepatic insufficiency/Liver failure Ascites Hypertension Diabetes Dialysis COPD Anti-platelet use Anticoagulant use Immunosuppression History of AAA Heart failure 0% (0) 0% (0) 45% (81) 18% (32) 0% (0) 8.2% (15) 10.4% (19) 6.6% (12) 23% (42) 0.55% (1) 0.55% (1) 0% (0) 0% (0) 57% (120) 27% (56) 0% (0) 4.8% (10) 9.1% (19) 10.9% (23) 11% (24) 0% (0) 2.38% (5) 0.18 1 0.032 0.013 1 0.16 0.64 0.13 0.002 0.28 0.14 55% (100) 54% (113) 0.82 Recurrent 1.6% (3) 2.9% (6) 0.42 Current active infection 3.9% (7) 2.4% (5) 0.4 History of MRSA infection
Operative Details CD (182) Hernia width (cm) (IQR) Approach Open Laparoscopic Robotic CDC class I II III IV Mesh Position Sublay Onlay Retromuscular Mesh type Permanent Synthetic Biologic/Other UC (210) 10 (5,15) 10 (4,15) 145 (80%) 12 (6%) 25 (14%) 160 (76%) 11 (5%) 32 (16%) 30 (16.5%) 85 (46.7%) 65 (35%) 2 (1.1%) 26 (12.4%) 106 (50.5%) 72 (34.3%) 6 (2.9%) 146 25 105 165 25 117 142 (83%) 40 (17%) 168 (88%) 42 (12%)
30 day outcomes Crohn s disease (N=182) Ulcerative Colitis (N=210) p-value 6 (3,9) 5 (3,8) 0.3 Length of stay , median in days (IQR) 14% ( 26) 13% ( 28) 0.79 Readmission 6.0% ( 11) 8.1% ( 17) 0.43 Reoperation 40% ( 72) 31% ( 65) 0.075 Postoperative medical complications (any) 12.1% ( 22) 8.2% (15) 4.3% (8) 1% (2) 8.1% ( 17) 6.2% (13) 1.9% ( 4) 0.5% ( 1) 0.19 0.57 0.39 0.71 Surgical site infection Superficial Deep Organ space 13% ( 24) 10% ( 22) 0.18 Surgical site occurrence 10% (19) 11% ( 24) 0.76 Surgical site infection/occurrence requiring procedural intervention
Surgeon Reported Hernia Recurrence CD (182) UC (210) <90 day recurrence 4/182 (2.2%) 1 midline 1 parastomal 2 unknown 7/57 (12.2%) 1 midline 3 parastomal 2 unknown 20/85 (23.5%) 2 midline 10 parastomal 8 unknown 8/210 (3.8%) 1 midline 4 parastomal 3 unknown 23/114 (20.2%) 1 midline 17 parastomal 5 unknown 44/170 (25.9%) 1 midline 33 parastomal 10 unknown 1 year follow up 4 year follow up
Reoperation Rates CD (136) UC (143) Total (279) Reoperation by 4 years 19 (14%) 29 (20.2%) 48 (17%)
Reoperation Reasons Reason for Reoperation N Major wound complications (3) All in CD patients 2/3 with enteroprosthetic fistulas Hernia recurrences past 90 days Early Recurrence within 90 days 13 12 Bowel obstruction 6 Major wound complication 3 Unrelated intra- abdominal pathology Unknown 3 11
HerQLes Scores HerQLes Baseline, median (IQR) 1 year, median (IQR) 2 year, median (IQR) 3 year, median (IQR) 4 year, median (IQR) CD 32 (17, 52) 65 (37,92) 60 (35, 87) 57 (42,87) 70 (52,90) UC 32 (13,53) 69 (36,84) 68 (30,83) 48 (35,68) 64 (35,84) 199 112 97 54 40 1 0.48 0.55 0.14 0.5
Conclusions 1. Parastomal hernias are challenging and carry a high complication/recurrence rate in patients with IBD 2. There doesn t appear to be any major differences in risk for PSH repair with CD compared to UC 3. The decision to repair PSH in these patients should be weighed heavily against the post- operative risk on an individualized basis