OPAL Team Improving Care for Frail Older Patients at Our Lady of Lourdes Hospital
Older Persons Assessment and Liaison (OPAL) team at Our Lady of Lourdes Hospital focuses on providing comprehensive geriatric assessment for frail older patients in the Emergency Department to improve outcomes and reduce avoidable admissions. The team's introduction led to positive results in patient care and discharge rates, with plans for further improvements through PDSA cycles.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
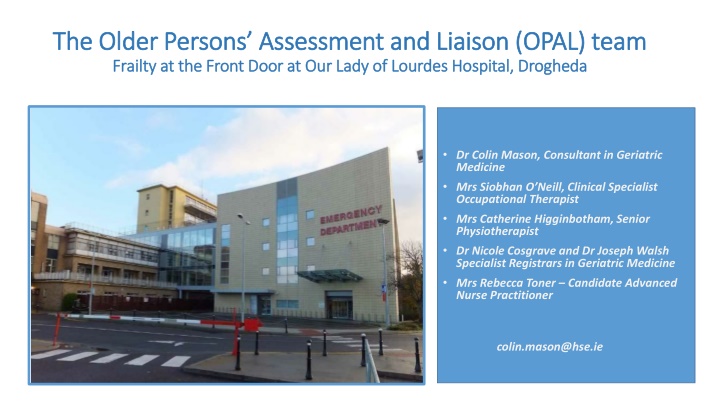
The Older Persons Assessment and Liaison (OPAL) team The Older Persons Assessment and Liaison (OPAL) team Frailty at the Front Door at Our Lady of Lourdes Hospital, Drogheda Frailty at the Front Door at Our Lady of Lourdes Hospital, Drogheda Dr Colin Mason, Consultant in Geriatric Medicine Mrs Siobhan O Neill, Clinical Specialist Occupational Therapist Mrs Catherine Higginbotham, Senior Physiotherapist Dr Nicole Cosgrave and Dr Joseph Walsh Specialist Registrars in Geriatric Medicine Mrs Rebecca Toner Candidate Advanced Nurse Practitioner colin.mason@hse.ie
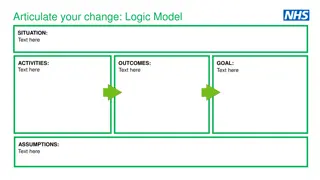
Background Older people frequently attend Emergency Departments (EDs). They often experience poorer outcomes, long stays and potentially avoidable admissions. There is evidence that teams who deliver Comprehensive Geriatric Assessment (CGA) can reduce admission rates and have positive effects on length of stay of older people in hospitals as a whole. While most EDs in Ireland have some model of CGA delivery, the most effective approach remains unclear. Aims We describe the recent introduction of a consultant-led multidisciplinary team in the ED of our hospital. The team aims to quickly recognise patients presenting with frailty syndromes and to deliver CGA effectively for those in whom it is felt that safe discharge can be achieved. Change initiative A baseline audit was performed in August 2021. In October 2021, the OPAL team commenced working and began screening patients and selectively delivering CGA in the ED 3 days a week. A further day was spent in virtual clinic reviewing patients discharged by the team. Measurements recorded include baseline patient demographics, Clinical Frailty Scores (CFS), time from screening to initiation of CGA, time taken to perform CGA, discharge rates among the patients who received CGA and their 7 and 30-day readmission rates.
PDSA Cycles PDSA 1.0 Initial baseline audit was in Summer 2021. The service commenced late October 2021. Initially a 3 day service with 1 day of virtual follow-up. We collaborated with the RCSI QI team. A Zoom meeting with a more well-established ED service was undertaken to compare and contrast our processes and to help guide best practice. PDSA 2.0 February 2022 Our Candidate ANP was repatriated. Temporary administrative support was put in place. Rapid Access Clinic commenced. An Excel master-sheet was set up to allow rolling data-analysis. A screening sticker is being introduced to prompt more rapid work-up of CGA-eligible patients. Clinical Governance meetings are planned. Further contact with similar teams are also planned to guide ongoing improvements in practice. PDSA 3.0 Planned for May 2022 when registered ANP and other staff in place. Increase to 4 day service along with the 1 day Rapid Access Clinic. Exploration of the introduction of a dedicated frailty assessment area as resources allow. Results The mean CFS of patients undergoing CGA was 5.7 (moderately frail, higher than expected). Mean time from screening to initiation of CGA was 38 minutes with a median of 15 minutes. The average time taken for CGA was just under 2 hours. The discharge rate of patients receiving CGA is currently 67% which compares favourably to similar studies in the literature. The readmission rate at 7 days is currently 0% with a 30 day readmission rate of 6%. No significant safety issues or complaints have been encountered to date. One formal letter of compliment was received from a patient s relative.
Average Time from Screening to onset of CGA (minutes) % of Patients Discharged CGA vs no CGA CGA No CGA Outcomes and Benefits to Patients The team has delivered safe and timely discharges of people who were otherwise likely to have undergone hospital admission. The readmission rate has been low. In the first 2 months, a possible saving of over 300 bed days has been made with potential for over 2000 bed days saved per year. Sustainability The recent introduction of a Rapid Access Clinic aims to improve the team s ability to provide more robust and effective CGA and interventions. A replacement ANP has been recruited. Additional posts have been approved to increase service capacity. When staffing improves, the team intends to work towards 5 days a week cover. The potential for a dedicated frailty admissions area has been identified in the hospital. In time, the project intends to develop links with outreach services in line with national integrated care strategy. What seems to have worked well A flattened team hierarchy. More timely and focused screening processes as experience and mutual understanding develops. Early starts (8am onwards) to screening. Regular team meetings with constant focus on improving processes.